Diabetes is a chronic condition that affects how the body regulates blood glucose levels, and recognising the signs of a diabetic emergency can save a life. In Australia, diabetic emergencies are common — Ambulance Victoria attended more than 41,000 cases of hypoglycaemia and hyperglycaemia over a seven‑year period, with numbers continuing to rise each year. Currently, more than 1.9 million Australians are living with diabetes, and over 300 people are diagnosed daily. Immediate first aid can prevent serious complications or death.
Whether it’s hypoglycaemia (low blood sugar) or hyperglycaemia (high blood sugar), knowing what to do — and acting quickly — is vital. This article explains what diabetes is, how to recognise the warning signs of a diabetic emergency, and the essential first aid steps to take in line with Australian guidelines.
First Aid Pro offers nationally recognised training to equip you with the skills to respond effectively to health crises. Enrol in a First Aid Course today and gain confidence in handling medical emergencies.

Key Takeaways
- Diabetes can cause life-threatening emergencies if blood sugar is too high or too low.
- Hypoglycaemia requires quick sugar intake if the person can swallow safely.
- Hyperglycaemia can develop slowly but may require urgent hospital care.
- First aid training helps you respond confidently to medical emergencies like diabetic crisis episodes.
- New technologies like Dexcom G7 help manage blood sugar levels but don’t replace first aid.

Understanding Diabetes – What Every First Aider in Australia Should Know
Diabetes – What Is It?
Diabetes is a chronic condition that affects how your body regulates blood glucose (sugar) levels. Normally, after you eat, carbohydrates are broken down into glucose, which enters your bloodstream. A hormone called insulin, produced by the pancreas, acts like a key to help move glucose from your blood into your body’s cells, where it’s used for energy.
For people with diabetes, this system does not work properly.
The body either:
- Does not make any insulin (or enough), OR
- Cannot use insulin effectively (insulin resistance).
This results in high levels of glucose remaining in the blood, which over time can damage blood vessels, nerves, kidneys, eyes, and increase the risk of heart disease.
Main Types of Diabetes
- Type 1 Diabetes: An autoimmune condition where the immune system destroys insulin-producing cells in the pancreas. People with type 1 diabetes make little or no insulin and require lifelong insulin injections. This usually appears in childhood or young adulthood but can develop at any age.
- Type 2 Diabetes: The most common form, often linked to genetic and lifestyle factors. The body becomes resistant to insulin and/or does not produce enough. It usually develops in adults but is increasingly diagnosed in young people. Can often be managed with healthy lifestyle changes, but may require medication or insulin as the condition progresses.
- Gestational Diabetes: Occurs during pregnancy when the body cannot cope with extra insulin needs. Although it usually goes away after birth, it increases the risk of developing type 2 diabetes later in life.
- Other Forms: Less common types include monogenic diabetes (due to a single gene change), diabetes from pancreatic disease, or medication-related diabetes.
Recognising and Managing Diabetes
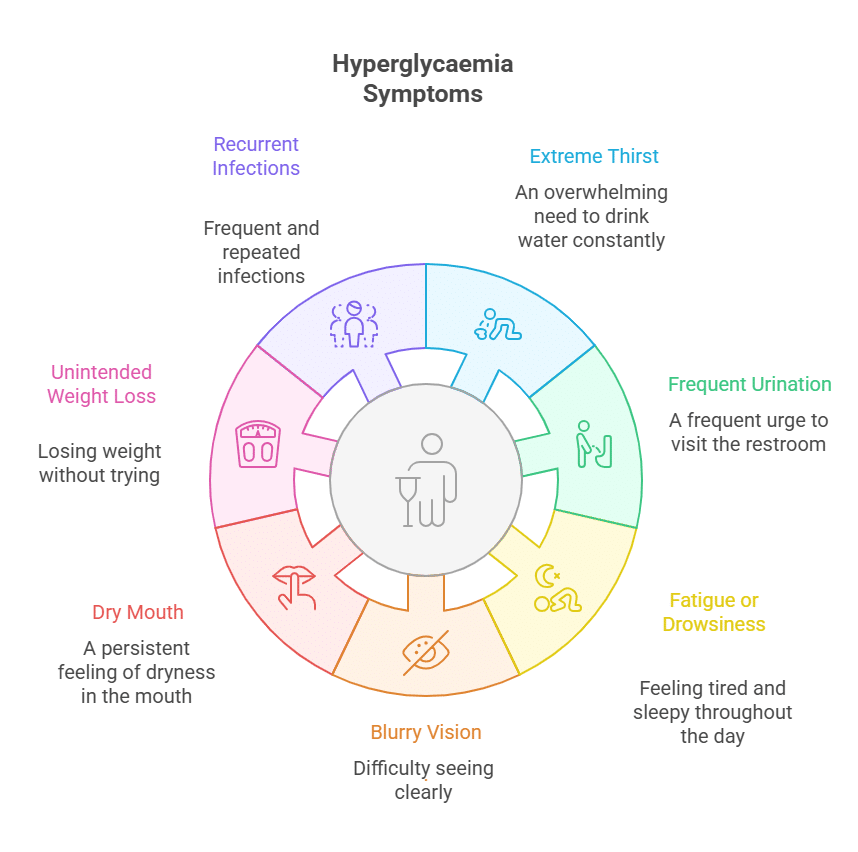
Common symptoms can include:
- Excessive thirst and frequent urination
- Fatigue
- Blurred vision
- Frequent infections and slow-healing wounds
Controlling blood glucose is essential to prevent both short- and long-term complications. Management may include a combination of diet, physical activity, medications, and regular blood glucose monitoring.
Diabetes in Australia
- Diabetes is one of Australia’s fastest-growing chronic diseases.
- More than 1.9 million Australians are living with diabetes.
- Early diagnosis, effective management, and regular medical care are crucial to preventing complications.

What Is Prediabetes?
Prediabetes means your blood glucose levels are higher than normal but not yet high enough to be classified as type 2 diabetes. It is an important warning sign—without intervention, about 1 in 3 people with prediabetes will develop type 2 diabetes within 10 years.
Prediabetes often has no obvious symptoms and is usually detected by blood tests (such as fasting glucose, HbA1c, or a glucose tolerance test).
Cause and Risk Factors For Prediabetes:
All risk factors for type 2 diabetes apply, particularly:
- Being overweight
- Physically inactive lifestyle
- High blood pressure or abnormal cholesterol
- Family history of diabetes
- Past gestational diabetes or PCOS
- Certain ethnic backgrounds
Prevalence in Australia (2025 Data)
Nearly 1 in 6 Australian adults (over 2 million people) over the age of 25 have prediabetes. This is a major risk for future type 2 diabetes and cardiovascular disease.
Screening and Prevention
- Screening: Those at high risk should have regular blood glucose checks. The Australian Type 2 Diabetes Risk Assessment (AusDRisk) tool is recommended for assessing risk, followed by pathology tests if indicated.
- Prevention: Lifestyle changes are shown to be effective:
- Weight loss (losing 5-10% of body weight)
- Healthy eating
- Physical activity (at least 150 minutes per week)
- Managing cholesterol and blood pressure
- Stopping smoking
Intensive lifestyle programs are the most effective intervention. Medication like metformin may be used on medical advice but is less effective than lifestyle change unless other risk factors apply.
The Main Types of Diabetes
Type | Cause | First Aid Consideration |
Type 1 Diabetes | Autoimmune destruction of insulin-producing cells in the pancreas. | People with type 1 diabetes depend on insulin injections or pumps. Emergencies often involve low blood sugar. |
Type 2 Diabetes | Body becomes resistant to insulin or doesn’t produce enough. | More common in adults, but increasingly in children. High and low blood sugar emergencies possible. |
Gestational Diabetes | Develops during pregnancy. | Risk of high blood sugar; emergencies less common but possible. |
Recognising the Signs of High and Low Blood Sugar

Hyperglycaemia and Hypoglycaemia: Key Differences and Definitions
What is Hyperglycaemia?
Hyperglycaemia (or hyperglycemia) means high blood glucose (sugar) levels. It most commonly refers to blood glucose levels that are above the normal range. While targets vary, hyperglycaemia is generally defined as:
- Fasting (no food for 8 hours): Above 6.9–7.0 mmol/L (125–126 mg/dL)
- After eating (2 hours): Above 10.0–11.1 mmol/L (180–200 mg/dL)
- Some clinical sources flag >15 mmol/L as severe hyperglycaemia
Causes:
- Most often seen in people with diabetes due to insufficient insulin, missed medications, infection, stress, or excessive carbohydrate intake.
Risks:
Persistent hyperglycaemia can cause serious long-term complications (nerve, kidney, eye, and heart damage). Very high levels can lead to life-threatening emergencies like diabetic ketoacidosis (especially in type 1 diabetes).
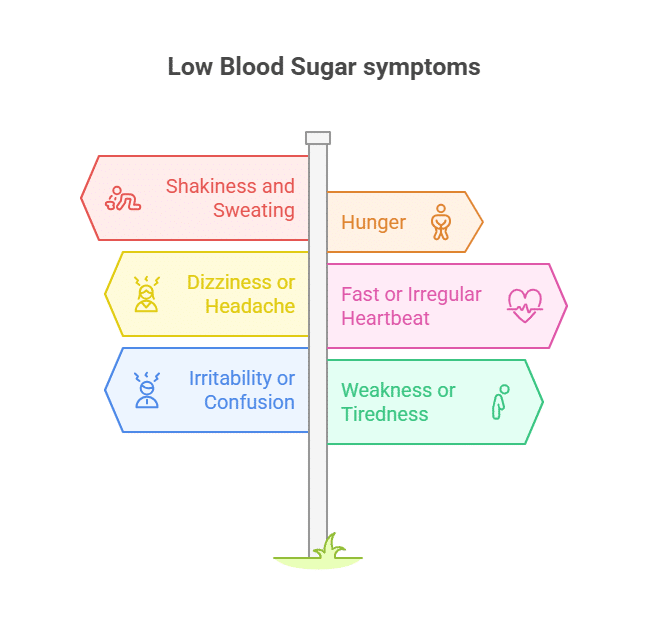
What is Hypoglycaemia?
Hypoglycaemia (or hypoglycemia) means low blood glucose (sugar) levels, typically:
- Below 4.0 mmol/L (72 mg/dL)
- Many guidelines define treatment thresholds at below 3.9 mmol/L (70 mg/dL)
Causes:
Most commonly a result of diabetes treatment (insulin or certain tablets), but can also be caused by:
- Skipping meals
- Excess alcohol intake
- More physical activity than usual
- Some rare medical conditions
Risks:
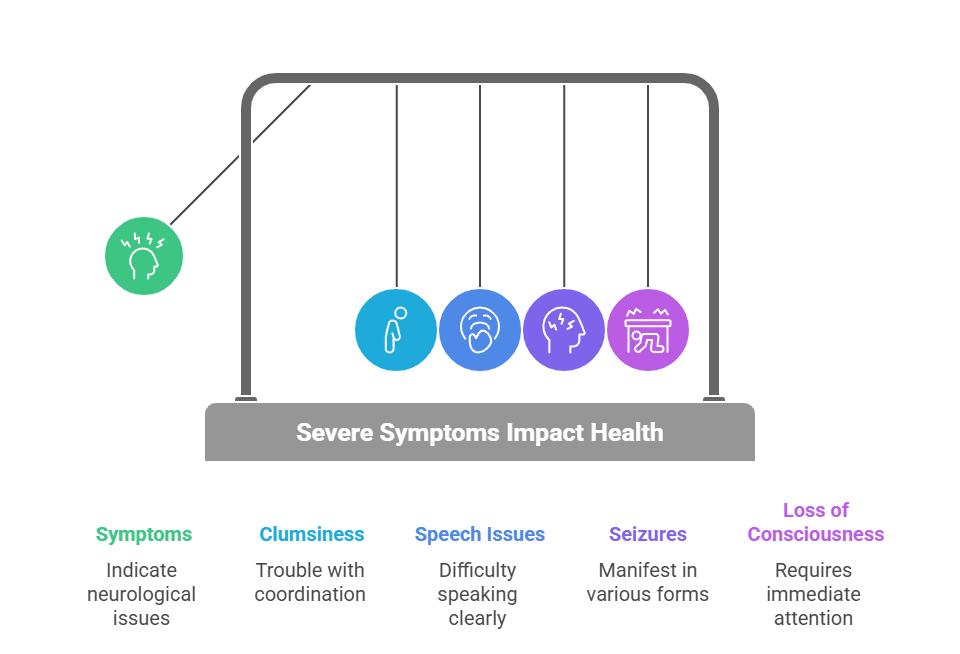
Hypoglycaemia can develop quickly and is considered a medical emergency—the brain depends on glucose. If not treated rapidly (with glucose—food or drink), it can result in coma or death.
First Aid Fact:
Hypoglycaemia can occur rapidly, especially in people using insulin or certain diabetes medications.

First Aid for Hypoglycaemia (Low Blood Sugar)
Quick recognition and treatment can prevent serious complications
- Sandwich
- Glass of milk
- Piece of fruit
- Small tub of non-diet yoghurt
- Place the person in the recovery position (side-lying)
- Do NOT give anything by mouth
- Monitor breathing and consciousness
Let the person manage it if they're able. First aiders should only focus on the hypoglycaemia treatment steps above.

First Aid for Hyperglycaemia (High Blood Sugar)
Recognising and managing elevated blood glucose levels
- Do NOT give anything by mouth
- Keep airway clear of any obstructions
- Monitor for breathing and consciousness
When Unsure if Blood Glucose is High or Low
If you are uncertain whether it is hypoglycaemia or hyperglycaemia, always treat as for hypoglycaemia (give sugar). This action can rapidly resolve low blood sugar and is unlikely to cause harm if levels are high.
Key Points to Remember
- Respond urgently—fast action in a diabetic emergency saves lives.
- Always call an ambulance (000) if:
- The person does not improve after treatment.
- Becomes unresponsive, cannot swallow, or has a seizure.
- Never give anything by mouth if the person is unconscious or cannot swallow safely.

Using Diabetes Technology and Medication in First Aid Scenarios
Continuous Glucose Monitoring – Dexcom G7 in Australia
The Dexcom G7 is the latest generation of continuous glucose monitoring (CGM) systems available in Australia. It is designed to provide real-time, accurate tracking of blood glucose levels for people living with diabetes, including type 1, type 2, and gestational diabetes, from age 2 and up.
How Dexcom G7 Works
- All-in-One Wearable Sensor: The G7 sensor is 60% smaller than the previous model (Dexcom G6), making it more comfortable and discreet to wear. It is worn on the upper arm or abdomen and continuously measures glucose levels from interstitial fluid just under the skin.
- Real-Time Readings: Glucose data is sent every few minutes, wirelessly and automatically, to a compatible device (such as a smartphone, smartwatch, or optional Dexcom receiver).
- No Finger Pricks Required: The system offers glucose monitoring without the need for routine finger-prick blood tests for calibration or daily management.
- Customisable Alerts: Users receive real-time alerts and alarms for high or low glucose levels—including predictive warnings for “urgent low” glucose events.
- Integration: Dexcom G7 can connect with insulin pumps such as the t:slim X2 and is compatible with many health apps, allowing for integration into broader diabetes management plans.

Key Features
- Fast setup: 30-minute warm-up for the sensor.
- Sensor lifespan: 10-day wear per sensor, with an additional 12-hour grace period to allow for flexibility in changing the device.
- Waterproof: Suitable for swimming, showering, and physical activity.
- Data Sharing: Users can share glucose trends in real-time with family or carers via the Dexcom Follow app, helping improve safety and support.
Subsidy and Access in Australia
- Government Subsidy: From 1 March 2025, the Australian Government is subsidising the Dexcom G7 sensors through the National Diabetes Services Scheme (NDSS) for eligible people with type 1 diabetes and some others with specific needs.
- Eligibility: Typically, people with type 1 diabetes or those on intensive insulin therapy who fulfill NDSS criteria can access subsidised devices. Check the NDSS website or with your diabetes healthcare provider for details.
Benefits for People with Diabetes
- Improved Management: The G7 helps users and clinicians make informed decisions, with evidence of better HbA1c outcomes, fewer hypoglycaemic and hyperglycaemic events, and more time spent within target glucose range compared to finger-prick testing.
- User-Friendly: Designed for easy self-insertion, intuitive operation, and minimal training, making it accessible for a broad range of people living with diabetes.
- Peace of Mind: Predictive and real-time alerts allow early intervention, potentially preventing severe highs and lows.

Semaglutide Medication and Treatment in Australia (2025)
Semaglutide is a glucagon-like peptide-1 receptor agonist (GLP-1 RA) used in Australia primarily for the treatment of type 2 diabetes and, more recently, chronic weight management and cardiovascular risk reduction in patients who are overweight or have obesity. It is marketed under the brand names Ozempic (mainly for type 2 diabetes) and Wegovy (for chronic weight management and cardiovascular risk reduction).
Availability and Brands
- Ozempic (Novo Nordisk): Used for type 2 diabetes management. As of June 1, 2025, new 3 mL pre-filled pens are PBS-listed, replacing the previous 1.5 mL version (which will be phased out by December 2025). The recent supply disruptions have eased, and patients should now be able to access Ozempic through pharmacies, though local shortages may persist temporarily.
- Wegovy (Novo Nordisk): Approved for weight management and, since December 2024, for reducing cardiovascular risk in adults with established cardiovascular disease and BMI ≥27 (without diabetes). However, Wegovy is not currently subsidised on the PBS and can be expensive out-of-pocket.
- Both formulations are once-weekly injectable pens, administered subcutaneously.

Treatment Guidelines and PBS Criteria
- Type 2 Diabetes: Ozempic is PBS-subsidised for adults with type 2 diabetes who meet specific initiation and continuation criteria. GPs must closely adhere to PBS restriction criteria—recent Department of Health and Aged Care investigations have highlighted inappropriate prescribing, stressing Ozempic should only be PBS-prescribed for diabetes and not off-label for weight loss.
- Weight Management/Cardiovascular Risk Reduction: Wegovy is approved for adults (and adolescents ≥12) with obesity (BMI ≥30, or BMI ≥27 with weight-related conditions). It is also approved for adults with cardiovascular disease (and BMI ≥27) without diabetes, following SELECT trial data. It is not PBS-funded for these uses.
- Dosage:
- Ozempic: Usual maximum 1 mg once weekly for diabetes.
- Wegovy: Start at 0.25 mg weekly, increase every four weeks, up to a maintenance dose of 2.4 mg weekly for weight management or cardiovascular risk reduction.
- Administration: Subcutaneous injection, once weekly, same day each week. Both products have similar administration techniques.

Side Effects and Safety
- Common adverse effects:
- Nausea, vomiting, diarrhea, constipation, and abdominal discomfort are the most frequent and tend to subside over time.
- Fatigue and headaches may also occur.
- Serious but rare risks:
- Pancreatitis, gallbladder disease, and potential risk of thyroid tumors (observed in animal studies but not confirmed in humans).
- Worsening of diabetic retinopathy in diabetes patients, and very rarely, kidney problems or severe allergic reactions.
- Monitoring: Close monitoring for gastrointestinal symptoms and rare serious complications is recommended, particularly during initial titration and in patients with pre-existing risk factors.
Get trained now — Join one of First Aid Pro’s nationally recognised first aid courses and be prepared for medical emergencies in any situation.
Preventing Diabetic Emergencies and First Aid Awareness
Diabetic emergencies, such as severe hypoglycaemia (low blood glucose) or hyperglycaemia (high blood glucose), can be life-threatening if not managed promptly. Prevention relies on a combination of self-management, structured education, preparation, and swift action when warning signs appear. Here are key steps and guidelines—based on Australian health recommendations—for preventing diabetic emergencies:
1. Follow Your Diabetes Care Plan
- Monitor blood glucose regularly according to your care team’s advice.
- Take medications as prescribed, including insulin or non-insulin therapies, and do not skip doses.
- Attend regular diabetes reviews and education sessions (these are available through the National Diabetes Services Scheme and are recommended annually) to update your knowledge and skills.
2. Healthy Lifestyle Choices
- Eat regular, balanced meals that align with your care plan. Do not skip meals.
- Stay physically active and track how exercise affects your blood glucose.
- Limit alcohol consumption and avoid binge drinking. Always eat if you drink alcohol, as it can trigger delayed hypoglycaemia.
- Do not smoke, as smoking increases the risk of complications.
3. Be Prepared for Emergencies
- Carry fast-acting glucose (e.g., glucose tablets, jellybeans, sweet drinks—not diet varieties) with you at all times, especially if you use insulin or medications that can lower blood glucose.
- Store a diabetes emergency kit with medications, glucose, snacks, a glucometer, spare batteries, and important contacts—especially important during travel or disasters.
- Wear diabetes identification (bracelet or necklace).

4. Personalised Emergency Plans
- Have a written diabetes management plan, especially if you live in disaster-prone areas or have complex medication regimens. Review and update your plan annually.
- Inform family, friends, teachers, and colleagues about your condition and what to do in case of an emergency.
- For children and adolescents, ensure caregivers and school staff are trained to recognise and respond to diabetic emergencies.
5. Infection and Illness
- Treat infections promptly, as infections can quickly worsen glucose control.
- Follow a “sick day” plan provided by your care team for managing diabetes during illness, which may involve more frequent glucose and ketone testing.
References
- Diabetes Australia – www.diabetesaustralia.com.au
- Australian Resuscitation Council Guidelines – www.resus.org.au
- American Diabetes Association – www.diabetes.org
- NDSS – www.ndss.com.au