Iron deficiency (low iron) is when your body doesn’t have enough iron to make healthy red blood cells. This guide explains symptoms and causes, how iron is a mineral used to make haemoglobin, the tests that diagnose iron deficiency, and the best treatment for iron deficiency including: dietary iron, iron supplement options, and, when needed, iron infusions—all in an Australian context.
Want practical skills to help if someone feels faint or dizzy? Enrol in a nationally recognised First Aid course with FirstAidPro.
Key Takeaways
- Iron deficiency is common and can exist without anaemia; check ferritin and iron studies if symptoms fit.
- Main causes: blood loss (e.g., heavy periods, GI), low dietary iron, malabsorption, and increased needs (pregnancy, teens, athletes).
- Treatment: improve dietary iron intake, optimise iron absorption, then use iron supplementation when indicated; consider iron infusions if tablets aren’t suitable.
- Prevention: plan meals with iron and vitamin C, time tea/coffee away from iron, and re-test to ensure the body’s iron stores are restored.
- Quick note: This article is educational, not medical advice. Always speak with your GP before you take iron supplements or change medicines.
Low Iron Explained: Iron, Iron Deficiency, and Iron Deficiency Anaemia
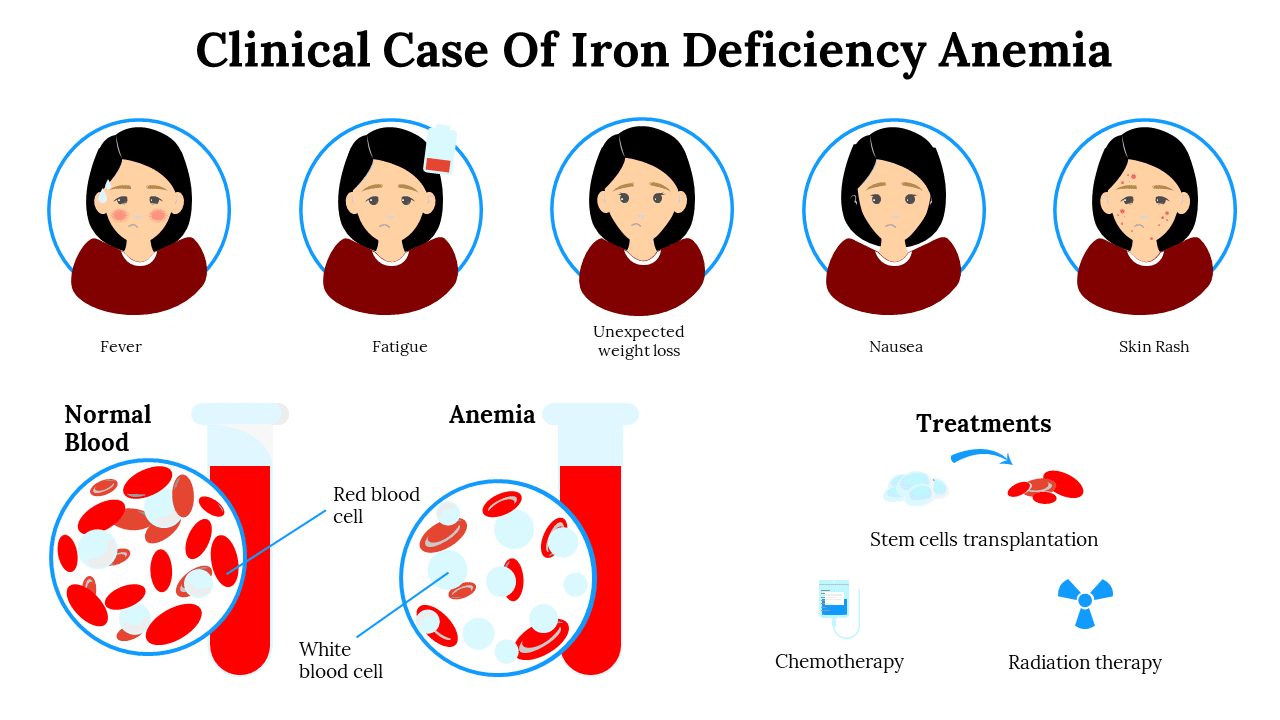
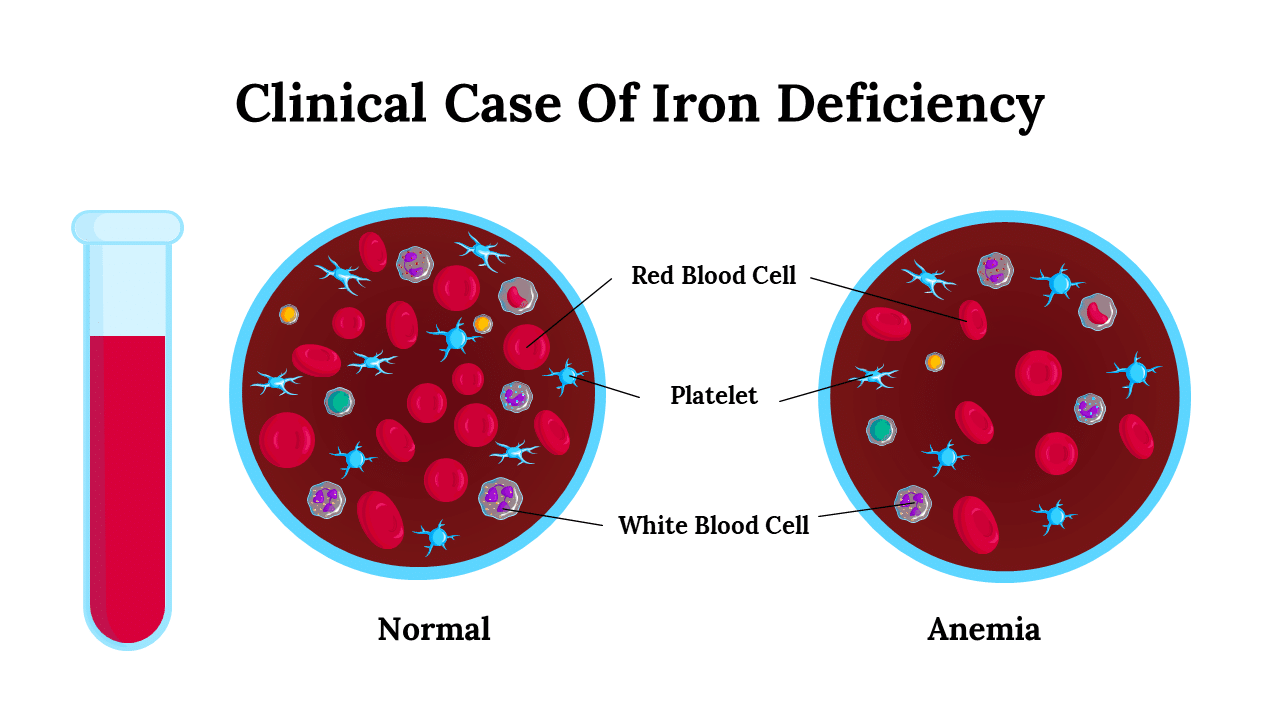
Iron is an essential nutrient for making hemoglobin, the protein in red blood cells that carries oxygen throughout the body. Without enough iron, the body cannot make healthy, oxygen-carrying red blood cells, leading to diminished organ function and energy levels.
Iron deficiency means body iron (your iron stores) is low; if it progresses and haemoglobin falls, you develop iron deficiency anaemia. You can be iron deficient (low ferritin) without anaemia, so testing matters.
Iron studies at a glance
Health professionals diagnose iron deficiency using iron studies, not just “serum iron”. Typical panels include:
- Ferritin (most useful indicator of iron stores),
- Transferrin saturation (TSAT),
- Total iron-binding capacity (TIBC)/transferrin,
- Haemoglobin and red cell indices (MCV/MCH).
Ferritin thresholds vary by setting and inflammation status; Australian guidance commonly uses thresholds <30 μg/L for deficiency in adults (lower in some labs), with higher cut-offs suggested if inflammation is present.

Symptoms of Iron Deficiency (Early to Severe)
People with low iron levels often notice:
- Tiredness/fatigue, poor concentration/brain fog, headaches
- Breathlessness, dizziness, or feeling faint
- Pale skin, cold hands/feet
- Hair loss or brittle hair; spoon nails (koilonychia)
- Restless legs; pica (craving/chewing ice or non-food items)
- Children/teens: behaviour changes, slower learning, reduced sport performance
Who’s at increased risk of iron deficiency?
- Women with heavy periods, pregnancy/postpartum, frequent blood donors
- Children and adolescents (growth), athletes (higher needs)
- People with low iron intake (some vegetarian/vegan patterns), malabsorption (coeliac disease, IBD, post-bariatric surgery), or medicines that reduce stomach acid (e.g., PPIs) or increase bleeding risk (e.g., NSAIDs)
What Causes Low Iron?
Symptoms & Causes: Where Low Iron Commonly Starts
- Heavy menstrual bleeding
- Gastrointestinal (GI) bleeding: ulcers, polyps, cancers
- Frequent blood donation
- Diets low in iron
- Limited haem iron from meat/poultry/seafood
- Poorly planned vegetarian/vegan diets
- Coeliac disease, inflammatory bowel disease
- Reduced stomach acid (PPIs)
- Dietary inhibitors: tea/coffee tannins, phytates
- Post-bariatric surgery
- Pregnancy and postpartum
- Adolescence (growth spurts)
- Endurance training and high training loads
“What’s the Lowest Iron Level?” (Interpreting Results Safely)
There isn’t a single “lowest iron” number for everyone. Ferritin is the key test, but it rises with inflammation, so a “normal” ferritin can hide deficiency. Many Australian clinicians use <30 μg/L to flag deficiency in adults; in inflammatory states, higher thresholds (e.g., <70 μg/L) may be used. TSAT <20% suggests low available iron. Decisions depend on your history and exam—see your GP.
Red flags—seek urgent care or medical advice promptly if you have: black or bloody stools, chest pain, shortness of breath at rest, collapse/fainting, or rapid heart rate with dizziness.
Diagnosing Iron Deficiency in Australia
| Start with your GP |
Serum iron alone is not diagnostic — rely on ferritin and full iron studies.
|
|---|---|
| Finding the cause |
|
| Children & teens |
|
| Safety & next steps |
Red flags: black/bloody stools, chest pain, severe breathlessness, fainting — call 000.
|
Treatment for Iron Deficiency (Step by Step)

1) Food first: build your dietary iron intake
Dietary iron comes in two forms:
Type of iron | Typical sources | Absorption | Notes |
Haem iron | Lean red meat, lamb, pork, chicken, fish | Higher | Less affected by inhibitors |
Non-haem iron | Legumes, tofu/tempeh, leafy greens, nuts/seeds, iron-fortified cereals | Lower | Boost with vitamin C foods |
Use the Australian Food Composition Database (AFCD) to check specific iron amounts in common foods. (Food Standards Australia New Zealand)
Boost Iron Absorption
- Citrus, berries, kiwi
- Capsicum, tomatoes
- Fermented foods (e.g., yoghurt, sauerkraut)
- Tea/coffee (tannins)
- Bran/wholegrain phytates
- Large calcium doses with iron
Tip: Have vitamin-C rich foods with non-haem iron, and keep tea/coffee to at least 1–2 hours away from iron-rich meals or supplements.
2) Iron supplementation (tablets/liquids)
If diet alone isn’t enough, your GP may recommend an iron supplement. Product, dose and schedule are individualised—especially if you have gut side-effects, inflammation, or complex conditions. Expect re-testing to confirm recovery and to replenish iron stores for 2–3 months after haemoglobin normalises.
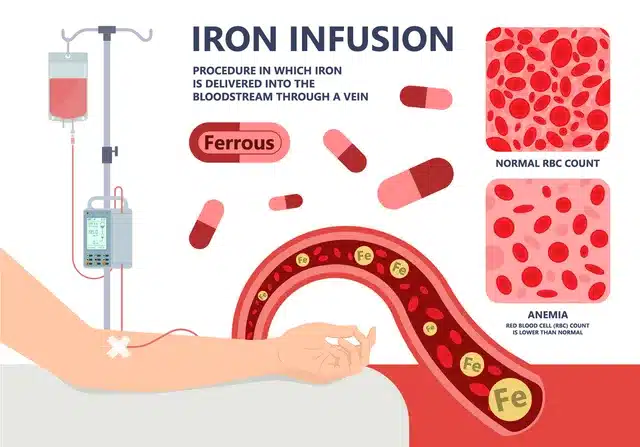
3) Iron infusions
An IV iron infusion is considered if oral iron fails, is not tolerated, or if rapid repletion is needed. Like any treatment, infusions carry risks (e.g., rare allergy; and with some products, low phosphate). Your clinician will weigh benefits and risks.
Build confidence in responding to symptoms of iron deficiency like dizziness or fainting—book HLTAID011 Provide First Aid with FirstAidPro today.
Low Iron in Specific Groups
| Women with heavy periods |
Consider tracking bleeding, discussing options (e.g., medical management), and planning re-tests to restore iron stores.
|
|---|---|
| Pregnancy |
Follow antenatal advice on supplements and timing with food; re-checks confirm adequate iron status for mum and baby.
|
| Children & teens |
Offer iron-rich foods (haem and non-haem) paired with vitamin C; your GP can advise dosing and follow-up bloods.
|
| Athletes |
Plan recovery nutrition around sessions; space tea/coffee from iron-rich meals or tablets to improve absorption.
|

Everyday Prevention: Keep Your Iron Levels Healthy
- Food sources of iron (practical examples)
Meal idea | Iron from food (type) | Absorption tip |
Beef stir-fry with capsicum & broccoli | Haem iron (meat) | Add vitamin-C veg; keep tea/coffee for later |
Lentil & tomato pasta | Non-haem iron (legumes) | Include lemon juice or salad with citrus |
Tofu & spinach curry with tomatoes | Non-haem iron | Pair with tomato & capsicum (vitamin C) |
Sardines on wholegrain toast, side of fruit | Haem iron (fish) | Fruit for vitamin C; avoid tea/coffee with the meal |
- Timing matters
Have tea/coffee away from iron-rich meals or tablets; consider spacing calcium supplements from iron. - Re-testing
If you were iron deficient, your GP will typically recheck haemoglobin and ferritin to confirm recovery and that body’s iron stores are restored.
Iron Deficiency – Knowledge Check
Iron Deficiency in Australia: Next Steps for Better Iron Health
Iron deficiency and iron deficiency anaemia are common—but fixable—when you act early. If symptoms fit, see your GP for ferritin and full iron studies (not serum iron alone). Tackle the cause, lift your dietary iron with haem and non-haem sources, optimise iron absorption (pair with vitamin C; time tea/coffee away), and use an iron supplement only as advised.
Re-test to confirm your iron stores have recovered, especially after pregnancy, heavy periods, growth spurts, or endurance training. Small, steady changes—plus the right treatment—restore energy and reduce the risk of relapse.
Build the skills to respond to dizziness, fainting and related first aid scenarios—enrol in a nationally recognised First Aid course with FirstAidPro today.
References
- Healthdirect: Iron deficiency—symptoms, causes, prevention & treatment. (Healthdirect)
- Better Health Channel (Vic): Iron and iron deficiency (food sources, absorption boosters/inhibitors). (Better Health Channel)
- MJA (2024): Updating the diagnosis and management of iron deficiency (cut-offs, evaluation, investigation pathways, monitoring). (mja.com.au)
- RCH Clinical Practice Guidelines: Iron deficiency in children (ferritin as key test; management). (Royal Children’s Hospital)
- NSW Health: General guide to iron and iron deficiency (consumer resource). (CEC Health NSW)
- FSANZ AFCD: Australian Food Composition Database (check nutrient values for Australian foods). (Food Standards Australia New Zealand)
Frequently Asked Questions
The content on this website offers general insights regarding health conditions and potential treatments. It is not intended as, and should not be construed as, medical advice. If you are facing a medical emergency, dial 000 immediately and follow the guidance provided.