Anaphylaxis is a severe, life-threatening allergic reaction that requires immediate first aid treatment with adrenaline and emergency medical attention. Understanding how to recognise the symptoms of anaphylaxis and respond quickly can save lives. In Australia, anaphylaxis cases have increased significantly over the past two decades, with food allergies affecting approximately 1 in 10 infants and 2 in 100 adults. The Australasian Society of Clinical Immunology and Allergy (ASCIA) provides evidence-based guidelines for the diagnosis and management of allergic reactions across Australia and New Zealand.
This comprehensive guide covers everything you need to know about allergic reaction first aid, from identifying early warning signs to administering life-saving emergency treatment. Whether you’re a parent, teacher, healthcare worker, or simply want to be prepared, this information could help you respond effectively when someone needs help.
Ready to gain life-saving skills? Enrol in nationally accredited Asthma and Anaphylaxis Training with First Aid Pro and learn hands-on techniques for managing severe allergic reactions. Our courses meet ASCIA standards and provide practical experience with adrenaline injectors.

Key Takeaways
- Anaphylaxis is a severe, life-threatening allergic reaction that requires immediate treatment with adrenaline
- Always give adrenaline first for suspected anaphylaxis – never delay to try antihistamines
- Call triple zero (000) immediately if someone is experiencing anaphylaxis
- Common triggers include food allergies, insect stings, medications, and latex
- Adrenaline injectors (EpiPen or Anapen) are the only first-line emergency treatment for anaphylaxis
- People with known asthma and allergy face increased risk of severe reaction

What Is an Allergic Reaction and How Does It Occur?
Understanding the Body’s Immune Response to Allergens
An allergic reaction occurs when the body’s immune system overreacts to a normally harmless substance called an allergen. In people with allergies, the immune system mistakenly identifies certain proteins – from foods, pollens, insect venom, medications, or other sources – as dangerous threats.
When someone with an allergy comes into contact with allergens, their immune system produces antibodies called Immunoglobulin E (IgE). These antibodies trigger specialised cells to release chemicals, including histamine, which cause the symptoms of an allergic reaction. This process can affect the skin, respiratory system, gastrointestinal tract, and cardiovascular system.
Mild to Moderate Allergic Reactions vs Anaphylaxis

Allergic reactions can range from mild to life-threatening. Understanding the difference is critical for appropriate first aid response.
Mild to moderate allergic reactions typically involve:
- Hives or welts on the skin
- Swelling of the face, lips, or eyes
- Tingling sensation in the mouth
- Abdominal pain or vomiting (after insect stings)
These symptoms affect only one body system and don’t involve breathing difficulties or a drop in blood pressure. While uncomfortable, mild allergic reactions don’t require adrenaline.
Anaphylaxis, also called a severe allergic reaction, is a medical emergency that involves:
- Multiple body systems (skin symptoms plus respiratory or cardiovascular symptoms)
- Sudden breathing difficulty or wheeze
- Swelling of the tongue or throat
- Sudden drop in blood pressure causing dizziness or collapse
- Loss of consciousness
Anaphylaxis can lead to death within minutes if untreated. The condition requires immediate treatment with adrenaline, followed by emergency medical care.
Signs and Symptoms of Anaphylaxis: What to Look For

Recognising anaphylaxis quickly is essential for effective emergency treatment. According to ASCIA guidelines, anaphylaxis should be suspected when someone has a known allergy and develops symptoms affecting their breathing or circulation.
Early Warning Signs of Allergic Reactions
The first symptoms of anaphylaxis often appear within minutes of allergen exposure, though reactions can sometimes be delayed by several hours. Early signs include:
- Tingling or itching of the lips, mouth, or throat
- Red, itchy rash (hives) appearing anywhere on the body
- Swelling of the face, lips, or eyes
- Stomach cramps, nausea, or vomiting
- A sense of impending doom or anxiety
Life-Threatening Symptoms of Anaphylaxis
The following symptoms indicate a severe reaction requiring immediate adrenaline administration:
Body System | Symptoms of Anaphylaxis |
Respiratory | Difficult or noisy breathing, wheeze, persistent cough, tight throat, hoarse voice, swelling of tongue |
Cardiovascular | Pale skin, floppiness (young children), dizziness, collapse, loss of consciousness |
Skin | Hives, swelling, redness (often present but not always) |
Gastrointestinal | Persistent vomiting, abdominal pain |
Critical warning: Someone with known asthma who is experiencing anaphylaxis may have particularly severe respiratory symptoms. These individuals face higher risk of fatal reactions.
How Quickly Symptoms Develop
Most anaphylactic reactions occur within 20 minutes to 2 hours after allergen exposure. However, the timeframe varies:
- Food-related reactions: Usually develop within minutes to 2 hours
- Insect sting reactions: Often occur within minutes
- Medication reactions: Can appear immediately or after several doses
Approximately 20% of people experiencing anaphylaxis will have a biphasic reaction – a second wave of symptoms occurring 4-12 hours after the initial episode. This is why emergency department observation is mandatory after anaphylaxis, even when symptoms improve.

🥜 Food Allergies That Cause Severe Reactions
Food allergies are the most common cause of anaphylaxis in Australian children. The “Big 9” allergens account for most food-related reactions:
| Allergen | Examples / Notes |
|---|---|
| Peanuts | Common trigger; rarely resolves; can cause anaphylaxis. |
| Tree nuts | Cashews, almonds, hazelnuts – often lifelong allergies. |
| Cow’s milk | Common in infants; some outgrow this allergy. |
| Eggs | Reactions range from mild to severe; often resolves with age. |
| Wheat | Can cause both allergy and coeliac-type sensitivities. |
| Soy | Common in processed foods and infant formulas. |
| Fish | Includes tuna, salmon, cod; often lifelong allergies. |
| Shellfish | Prawns, crabs, lobster – frequent adult trigger of severe reactions. |
| Sesame | Increasingly recognised; mandatory labelling in Australia. |
According to Anaphylaxis Australia and the National Allergy Council, peanut and tree nut allergies are particularly concerning because they rarely resolve and often cause severe reactions.
🐝 Insect Stings and Bites: Australian Risks
Australia’s unique insect population presents specific allergy risks. Allergies to insect stings affect approximately 3% of adults:
- Bee stings: Honeybees and native bees
- Wasp stings: European and paper wasps
- Jack jumper ants: Found in Tasmania and parts of mainland Australia; cause particularly severe reactions
- Tick bites: Can trigger mammalian meat allergy and immediate allergic responses
💊 Medication and Latex Allergies
Some individuals experience allergic reactions to medications or latex products. Common medication triggers include:
| Trigger | Examples / Risk Notes |
|---|---|
| Antibiotics | Penicillin and related drugs frequently cause allergic reactions. |
| Aspirin / NSAIDs | Can trigger hives, swelling, and respiratory distress. |
| Anaesthetic agents | Rare, but potentially life-threatening reactions may occur. |
| Contrast dyes | Used in medical imaging; can cause immediate allergic response. |
| Latex | Found in gloves, equipment, balloons; risk to healthcare workers and surgical patients. |
Natural rubber latex exposure can lead to skin irritation or anaphylaxis in sensitive individuals.

When you suspect someone is experiencing anaphylaxis, follow the ASCIA first aid plan for anaphylaxis:
| Step | What to do |
|---|---|
| Step 1 |
Lay the person flat – do not let them stand or walk.
|
| Step 2 |
Give adrenaline injector (EpiPen or Anapen).
|
| Step 3 |
Call Triple Zero (000) for an ambulance.
|
| Step 4 |
Give further adrenaline after 5 minutes if no response.
|
| Step 5 |
Contact the emergency contact person.
|
| Step 6 |
Transfer to an emergency department for at least 4 hours of observation.
|
How to Use an Adrenaline Injector (Autoinjector)
Adrenaline (also called epinephrine) is the only first aid treatment that can reverse severe allergic reaction (anaphylaxis). In Australia, two types of adrenaline injectors are available: EpiPen and Anapen.
EpiPen Administration:
- Form a fist around the device (orange end down)
- Remove the blue safety cap by pulling straight up
- Place orange end firmly against outer mid-thigh (at right angle)
- Push down hard until you hear a click
- Hold firmly for 3 seconds
- Remove and massage injection area for 10 seconds
- Note the time of injection
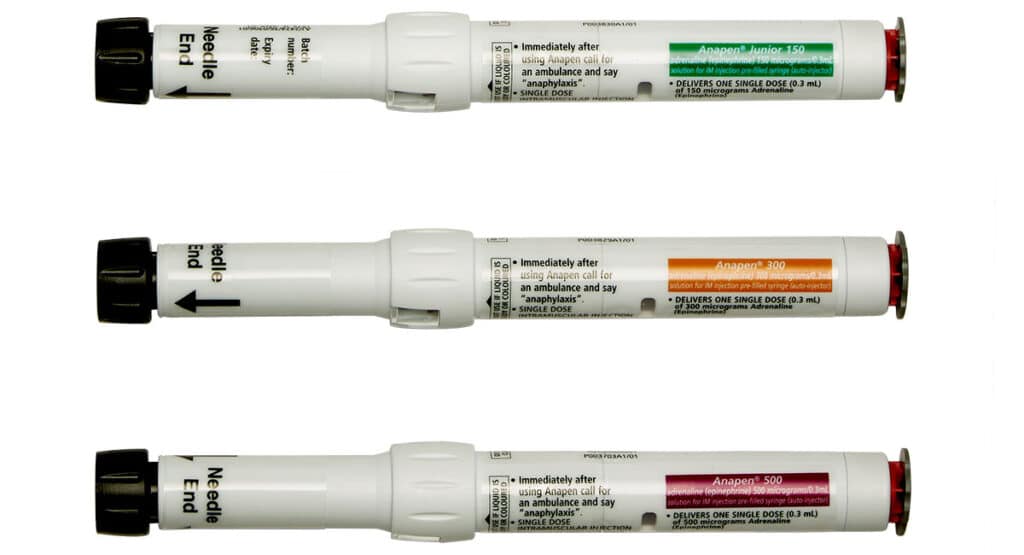
Anapen Administration:
- Pull off black needle cap
- Place black end firmly against outer mid-thigh (at right angle)
- Press red button – you’ll hear a click
- Hold for 10 seconds
- Remove and massage injection area for 10 seconds
You can inject through clothing if necessary. Don’t put your thumb over the end of the device or hold it with your fist wrapped around both ends.
Want to practice with trainer devices? First Aid Pro’s nationally accredited training includes hands-on experience with adrenaline injector trainers, so you’ll feel confident in an emergency. Our courses cover both EpiPen and Anapen systems.
- Call 000 Someone is experiencing anaphylaxis
- Call 000 You’ve administered adrenaline
- Call 000 You’re unsure if the reaction is severe
- Call 000 Someone with known asthma and allergy is having breathing difficulty
- The person is having an allergic reaction (say “anaphylaxis”)
- Your exact location
- Whether adrenaline has been given
- The person’s response to treatment

Anaphylaxis Training: Why First Aid Education Matters
Who Should Complete Anaphylaxis First Aid Training?
The management of anaphylaxis requires specific knowledge and practical skills. ASCIA recommends training for:
- Parents and family members of children with food allergies or insect sting allergies
- Teachers and school staff at schools with students at risk
- Early childhood educators in childcare centres
- Food service workers in restaurants and cafés
- Workplace first aiders in any setting
- Healthcare workers and allied health professionals
- Sports coaches and recreation staff
- Outcome Recognition of symptoms of anaphylaxis and mild allergic reactions
- Outcome Understanding ASCIA action plans and how to follow them
- Outcome Practical training on how to use an autoinjector correctly
- Outcome Positioning techniques for anaphylaxis patients
- Outcome When and how to administer CPR if required
- Outcome Legal protections for first aid providers in Australia
- Outcome Prevention strategies and allergen management

Allergic Reaction Risk Factors: Who Is Most at Risk?
Children and Anaphylaxis: Special Considerations
Australia has one of the highest rates of food allergies in the world, affecting approximately 10% of infants. Children face particular risks:
- Young children may not recognise or communicate symptoms clearly
- First reactions can occur without previous mild reactions
- School and social settings increase exposure risk
- Someone with known asthma faces higher risk of severe reactions
Schools must have action plans for students with allergies and anaphylaxis, including readily accessible adrenaline injectors and trained staff.
Adults with New-Onset Allergies
While food allergies typically develop in childhood, adults can develop new allergies at any age. Common adult-onset allergies include:
- Shellfish allergies
- Insect sting allergies
- Medication allergies
- Occupational allergies (latex, flour dust, chemicals)
Adults who develop sudden breathing difficulty or other severe symptoms after eating, being stung, or taking medication should get emergency medical attention immediately.
People with Asthma and Allergic Reactions
Having asthma significantly increases anaphylaxis risk. The combination of known asthma and allergy requires extra vigilance:
- Respiratory symptoms may be more severe
- Fatal reactions are more common in people with asthma
- Quick access to both asthma reliever puffer and adrenaline injector is essential
- Never delay adrenaline to use asthma medication first
If someone with known asthma and allergy develops breathing problems during an allergic reaction, treat as anaphylaxis and give adrenaline immediately.
All anaphylaxis cases require emergency department observation for at least 4 hours because:
- Symptoms can recur (biphasic reactions)
- Medical staff can monitor cardiovascular and respiratory function
- Additional treatment may be needed
- Proper diagnosis ensures appropriate follow-up
- Referral to an allergy specialist or clinical immunology and allergy physician
- Prescription for adrenaline injectors (at least two)
- An ASCIA action plan for anaphylaxis
- Information about allergy testing if the trigger is unknown
ASCIA action plans are standardised, evidence-based documents that guide emergency treatment. These plans include:
- Person's photo, name, and known allergies
- List of allergens to avoid
- Symptoms of anaphylaxis specific to that person
- Step-by-step first aid instructions
- Emergency contact details
- Doctor's signature and date
- Displayed prominently at home, school, and work
- Updated annually or when circumstances change
- Accompanied by in-date adrenaline injectors
- Understood by caregivers, teachers, and co-workers
Download ASCIA action plans free from the ASCIA website www.allergy.org.au.
People prescribed an adrenaline injector must carry it everywhere, every day:
- Always carry two autoinjectors – one dose may not be sufficient
- Check expiry dates monthly and replace before expiration
- Store at room temperature (not in cars or direct sunlight)
- Keep in original packaging to protect from light
- Take on holidays, day trips, and social events
Consider wearing medical alert jewellery that identifies your allergy and states you've been prescribed an adrenaline injector.
Allergen avoidance is the primary prevention strategy:
- Read all ingredient labels carefully
- Ask about ingredients when dining out
- Inform restaurant staff about severe allergies
- Carry safe snacks when travelling
- Teach children to never share food
- Wear closed shoes outdoors
- Avoid scented products that attract insects
- Stay calm around bees and wasps
- Consider venom immunotherapy (ask your doctor)
- Inform all healthcare providers about medication allergies before treatment
- Wear medical alert identification
- Educate family, friends, and colleagues about your allergies
Build your confidence in managing allergies and anaphylaxis. First Aid Pro offers comprehensive, nationally accredited training that goes beyond basic awareness. Learn practical skills including how to use an autoinjector, recognise symptoms, and respond effectively. Enrol in our Asthma and Anaphylaxis course.

First Aid Kit Essentials for Allergic Reaction
Homes, workplaces, and schools where people with allergies spend time should have allergy-specific emergency supplies:
Essential Items | Purpose |
Two adrenaline injectors | Primary treatment for anaphylaxis |
ASCIA action plan | Step-by-step emergency instructions |
Antihistamine tablets | Mild allergic reactions only (never for anaphylaxis) |
Asthma reliever puffer | For people with known asthma |
Emergency contact card | Names and phone numbers |
Mobile phone | To call triple zero |
Remember: antihistamines do NOT treat anaphylaxis. Always give adrenaline first for severe reactions, then call triple zero, then consider antihistamines only if prescribed for mild symptoms.
Allergic Reaction First Aid Training Saves Lives
The key messages for effective allergic reaction first aid are straightforward: recognise the signs of anaphylaxis affecting breathing or circulation, always give adrenaline first for severe reactions, lay the person flat, call triple zero immediately, and ensure follow-up with emergency services and allergy specialists.
For people living with allergies and anaphylaxis, proper management includes carrying two in-date adrenaline injectors everywhere, having an ASCIA action plan, wearing medical identification, and educating those around you about your condition.
Whether you’re a parent of a child with food allergies, a teacher, healthcare worker, or simply someone who wants to be prepared, getting trained in first aid for anaphylaxis gives you the knowledge and confidence to respond effectively in emergencies.
The Australasian Society of Clinical Immunology (ASCIA), Anaphylaxis Australia, and the National Allergy Council, offer action plans, educational materials, and support for people affected by allergies.
Don’t wait until an emergency occurs to learn these life-saving skills.
Take action today. Enrol in nationally accredited Asthma and Anaphylaxis Training with First Aid Pro and gain the practical skills and confidence to manage severe allergic reactions. Our courses are recognised across Australia, taught by experienced instructors, and include hands-on practice with adrenaline injector trainers. Your training could save a life.
References
- Australasian Society of Clinical Immunology and Allergy (ASCIA). (2023). ASCIA Guidelines for Schools, Preschools and Childcare.
- Australasian Society of Clinical Immunology and Allergy (ASCIA). (2024). ASCIA Action Plan for Anaphylaxis.
- Anaphylaxis Australia. (2024). Living with Anaphylaxis: Information and Support. www.allergyfacts.org.au
- National Allergy Council. (2023). Resources: Anaphylaxis
- Australian Resuscitation Council. (2023). Guideline 9.2.7 – Anaphylaxis.
- Therapeutic Goods Administration. (2024). Adrenaline Autoinjectors. Australian Government Department of Health. www.tga.gov.au