Blood thinners are medicines that reduce your blood’s ability to clot, helping prevent blood clots from forming in your veins, arteries, heart, or lungs. They don’t literally “thin” blood; instead they change the way your blood clots so you’re less likely to develop a clot that could cause a stroke, heart attack, DVT or PE.
Build confidence to recognise red-flag bleeding and respond safely. Enrol in a nationally recognised First Aid Course (HLTAID011) with First Aid Pro.

Key takeaways
- Blood thinners are medicines that help prevent blood clots but increase your risk of bleeding — know your red flags.
- Warfarin needs regular blood tests (INR) and steady vitamin K intake; DOACs usually don’t need INR checks.
- Never stop your blood thinner or change dose unless your clinician says so (including before a medical procedure).
- Tell every clinician you’re on an anticoagulant/antiplatelet and wear a medical alert bracelet or carry a card.
- If in doubt, talk to your doctor or pharmacist; in an emergency or severe bleeding, call 000.
Ready to go further? For workplaces or carers who need deeper capability, step up to Advanced First Aid (HLTAID014) with First Aid Pro.

What Are Blood Thinners?
A blood thinner (anticoagulant or antiplatelet) is a medication you take to help prevent blood clots if your risk for blood clots is raised — for example with atrial fibrillation, after some medical procedures (like stents), or after a previous blood clot.
Anticoagulant medicines (like warfarin and direct oral anticoagulants such as apixaban, rivaroxaban, dabigatran, and edoxaban) stop the blood from clotting by affecting the body chemicals (clotting factors) that help form blood clots, while antiplatelet medicines (like aspirin and clopidogrel) stop blood cells called platelets from sticking together and forming clots.
Breakdown
Anticoagulants target chemicals in your blood that are needed for clot formation.
Antiplatelets prevent blood cells called platelets from sticking together, so clots are less likely to form
How blood thinners work

As discussed, anticoagulants interfere with chemical steps in the clotting cascade so a fibrin clot is less likely to form. Antiplatelets help prevent blood cells called platelets from sticking together at a damaged blood vessel wall. Both help keep blood flowing but increase your risk of bleeding as a side effect. Do not stop taking your medicine unless your clinician tells you to.
Coagulation vs Platelets — How Blood Thinners Work
Blood thinners don’t literally “thin” blood — they reduce clot formation. Anticoagulants act on the coagulation cascade; antiplatelets act on the platelet plug.
Monitoring: Warfarin needs regular INR tests & steady vitamin K intake; DOACs usually don’t need INR checks (kidney review applies).
Monitoring: No INR; check interactions (some PPIs with clopidogrel) and follow cardiology advice.
| Key Differences | Anticoagulants | Antiplatelets |
|---|---|---|
| Primary action | Blocks clotting factors (cascade) | Blocks platelet activation/aggregation |
| Typical examples | Warfarin, Apixaban, Rivaroxaban, Dabigatran | Aspirin, Clopidogrel, Ticagrelor, Prasugrel |
| Monitoring | Warfarin → INR; DOACs → periodic renal review | No INR; interaction checks as advised |
| Common indications | AF stroke prevention; DVT/PE | Post-stent dual therapy; vascular disease |
Who might take blood thinners?

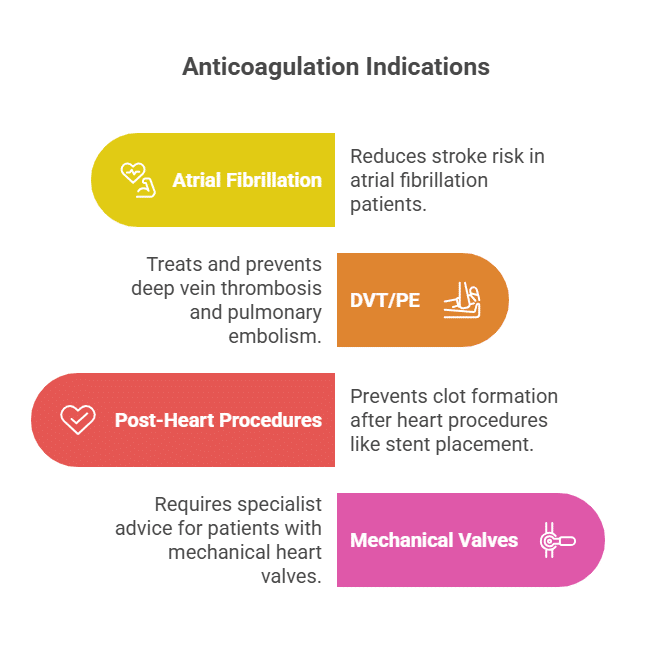
People who might take blood thinners are those at risk of forming dangerous blood clots or who already have certain heart or blood vessel conditions. Common reasons include having an irregular heartbeat (like atrial fibrillation), a history of heart attack or stroke, a heart valve replacement, a past blood clot, or recovering from surgeries such as hip or knee replacements.
Typical Groups Who May Need Blood Thinners
- People with atrial fibrillation (an abnormal heart rhythm) to prevent strokes.
- Those with artificial heart valves or certain congenital heart problems.
- Patients who have had or are at risk of deep vein thrombosis (DVT), pulmonary embolism, heart attacks, or strokes.
- Individuals recovering from surgery, especially hip or knee surgery, to prevent clotting during recovery.
- People with a history of blood clots or certain blood disorders.
- Some cancer patients and pregnant women with certain clotting risks may be prescribed blood thinners.
Special Considerations
- The decision to use blood thinners depends on multiple factors like age, pregnancy, bleeding risk, and other health conditions.
- These medicines help prevent clots but also increase the risk of bleeding, so they must be used under medical supervision.
Common reasons a clinician may prescribe a blood thinner include:
Helpful next step: Learn the first response for chest pain, fainting, and bleeding emergencies. Book Provide First Aid or CPR (HLTAID009) with First Aid Pro.

Warfarin vs newer oral anticoagulants vs antiplatelets
Warfarin remains widely used but needs regular blood tests (INR) and consistent vitamin K intake; newer blood thinners (often called DOACs or direct oral anticoagulants) usually don’t need regular blood work. Antiplatelets are different again (more common after stents). Your clinician will balance benefit (prevent clots) vs risk of bleeding.
Warfarin
An older anticoagulant that blocks vitamin K, needed for clotting.
Requires regular blood tests (INR monitoring) and frequent dose changes.
Has many drug and food interactions and increases the risk of bleeding.
Still preferred for some conditions (like mechanical heart valves and antiphospholipid syndrome), where newer drugs may not be as effective.
Newer Oral Anticoagulants (DOACs/NOACs)
Include apixaban, rivaroxaban, dabigatran, and edoxaban.
Offer predictable dosing with fewer food and drug interactions.
Require little to no regular blood monitoring.
Associated with lower risks of stroke, recurrent clot, and major bleeding compared to warfarin in most people.
DOACs may not work as well as warfarin for patients with certain rare conditions like antiphospholipid syndrome.
Antiplatelets
Include aspirin and clopidogrel and work by preventing platelets from sticking together.
Used mainly for heart attack and stroke prevention in people with arterial disease, not for treating clots like DVT or atrial fibrillation.
Usually have a lower bleeding risk compared to both warfarin and DOACs, but are less powerful against certain types of clots.
| Class | How they work | Examples | Monitoring | Food/Alcohol notes | Typical blood thinner use |
|---|---|---|---|---|---|
| Warfarin (anticoagulant) | Blocks vitamin-K dependent clotting factors | Warfarin | INR checks; dose adjusted to target range | Keep vitamin K intake consistent; alcohol in moderation per clinician | AF, DVT/PE, some valves |
| DOACs (anticoagulant) | Directly inhibit Xa or IIa | Apixaban, Rivaroxaban, Dabigatran, Edoxaban | No routine INR; kidney checks | Fewer food interactions than warfarin; follow product guidance | AF, DVT/PE (indication-specific) |
| Antiplatelets | Reduce platelet aggregation | Aspirin, Clopidogrel, Ticagrelor | No INR | Interaction checks (e.g., some PPIs with clopidogrel); alcohol moderation | After stents, certain vascular disease |
What’s new? Recent analyses suggest clopidogrel may outperform low-dose aspirin for some people with coronary artery disease; guidance may evolve. Always talk to your doctor before changing anything.
Side Effect Profile & Red Flags — Blood Thinners
All blood thinner pills raise the risk of bleeding. Know the red flags, when to call 000, and when to speak with your doctor or pharmacist.
Red flags — call 000 or go to ED
-
Severe, persistent, or unexplained bleeding — including vomiting blood, blood in your urine, or black stools.
-
Significant head knock while you’re taking a blood thinner — even if you feel okay at first.
-
Dizziness, weakness, or shortness of breath with bleeding.
If in doubt, seek urgent care. Do not self-stop or adjust doses without medical advice.
Everyday minor side effects
-
Easy bruising (minor).
-
Nosebleeds (minor).
If you’re worried, call your doctor or speak with a pharmacist for advice.
Vitamin K and taking warfarin safely

Vitamin K is important for blood clotting, and warfarin works by blocking vitamin K’s role in producing clotting proteins. If a person takes warfarin and suddenly eats a lot more vitamin K (from foods like green leafy vegetables), this can make warfarin less effective—meaning the blood may clot too easily and increase the risk of dangerous clots. On the other hand, cutting out vitamin K unexpectedly can make warfarin too powerful and raise the risk of bleeding.
What does INR stand for?
INR stands for International Normalised Ratio. In the context of blood thinners, it is a blood test that shows how long it takes for blood to clot, and is especially used to monitor people taking warfarin. The INR helps doctors make sure the warfarin dose is just right—too high means the blood clots too slowly (risk of bleeding), while too low means it clots too fast (risk of dangerous clots).
Key Safety Tips
- Keep vitamin K intake consistent: Eat similar amounts of vitamin K-rich foods each week rather than making big changes in the diet.
- Let your doctor know about major diet changes or supplements, as these can affect warfarin’s action and your INR levels.
- If INR levels get too high, doctors may use vitamin K itself as an “antidote” to help the blood clot again and reduce bleeding risk.
Staying consistent with vitamin K helps warfarin work safely.
Interactions, procedures and travel
- OTC pain relief: Many people on anticoagulants should avoid NSAIDs unless advised (interaction-bleeding risk). Always talk to your doctor or pharmacist.
- Before a medical or dental procedure: Your team might modify or temporarily stop your blood thinner; never do this yourself.
- Long trips: Move regularly, stay hydrated, and follow your clinician’s guidance to help prevent blood clots on flights.
- Alcohol: Discuss limits with your clinician, especially on warfarin where alcohol can affect INR.
Using Blood Thinners Safely — Quick Checklist
Tick these steps to take blood thinners safely and reduce your risk of problems.
- Always take your blood thinner as directed; don’t stop taking it without medical advice.
- Book your regular blood tests to check INR if you take warfarin.
- Keep vitamin K intake steady; don’t chase “zero vitamin K” diets.
- Tell every clinician you see that you’re taking a blood thinner (and wear a medical alert bracelet / carry a card).
- Watch for effects of blood thinners such as bleeding and call your doctor if unsure.
Time to Upskill: Prepare for emergencies linked to using blood thinners (falls, cuts, nosebleeds). Enrol in nationally certified first aid and CPR (HLTAID009) with First Aid Pro.
Blood Thinners – Knowledge Check
Answer the five questions below, then choose Check answers. Brand colours applied; fully mobile-friendly.
Using Blood Thinners (Anticoagulants) Safely
Blood thinners are highly effective at helping prevent blood clots, but they also carry a risk of bleeding. The safest approach is simple: take your blood thinner as directed, keep vitamin K intake steady if you take warfarin, attend any regular blood tests, and talk to your doctor or pharmacist before making changes or adding new medicines or supplements.
If you notice red-flag side effects—such as vomiting blood, black stools, or blood in your urine—seek urgent care and call 000. For routine questions about anticoagulant use, dosage timing, travel, or medical procedures, always ask your clinician first.
Used wisely and monitored well, blood thinner pills can reduce your chance of stroke, heart attack, and other clot-related emergencies while keeping you safe day to day.
Important Reminder
This article is general information for Australia and does not replace personalised medical advice. Always take your blood thinners as directed and talk to your doctor before you stop your blood thinners or change how you use it. If you experience heavy or uncontrolled bleeding, call 000 immediately.
References
- Queensland Health – Guideline for Warfarin Management in the Community (Australian INR and safety guidance)
- NHS – Anticoagulant medicines (how they work, taking them safely, interactions, duration).
- HealthyWA – Your lifestyle choices with warfarin (INR, alcohol, diet). (HealthyWA)
- NPS MedicineWise – Warfarin and how to take it (Australian consumer info, side effects).
- Guy’s & St Thomas’ NHS – Direct oral anticoagulants (patient overview, alert card).
- North Tees & Hartlepool NHS – Anticoagulants (Blood Thinners) (plain-English use cases).
- NICE NG196 – AF diagnosis & management (when anticoagulants are offered).
- Heart Foundation (AU) – Downloadable patient resources (cardiovascular context).