Understanding Swallowing Disorders And Dysphagia Support
Dysphagia is the medical term for difficulty swallowing. People with dysphagia have trouble moving food or liquid from the mouth to the esophagus and down to the stomach. Symptoms can include: sensation of food being stuck in the throat or chest, coughing or gagging while swallowing, pain while swallowing, regurgitation of food and choking on food.
Dysphagia can range from mild discomfort to a complete inability to swallow, and it can lead to serious complications such as malnutrition, dehydration, and aspiration pneumonia
Dysphagia affects thousands of Australians and requires specialised swallowing therapy from trained professionals. For NDIS providers and support workers, understanding how to manage swallowing disorders is a critical skill that directly impacts client safety and quality of life.
This article explores the essential components of dysphagia support training specifically tailored for NDIS and healthcare professionals working in high-intensity support environments.
First Aid Pro’s NDIS-recognised dysphagia support training program will equip you with the essential skills to safely manage swallowing disorders, prevent serious complications, and provide dignified, person-centered care. Don’t wait until an emergency occurs— Enrol now to build your confidence and competence in this critical high-intensity support skill.

he Need For Effective Dysphagia Treatment Strategies
Proper dysphagia management training ensures that clients receive appropriate care while reducing risks such as choking, malnutrition, and aspiration pneumonia. Within the NDIS framework, this training falls under high-intensity support skills, requiring specific certification and ongoing professional development.
Swallowing disorders can develop from various conditions including stroke, brain injury, Parkinson’s disease, cerebral palsy, and age-related changes. These disorders affect the complex process of moving food and liquid safely from the mouth to the stomach.
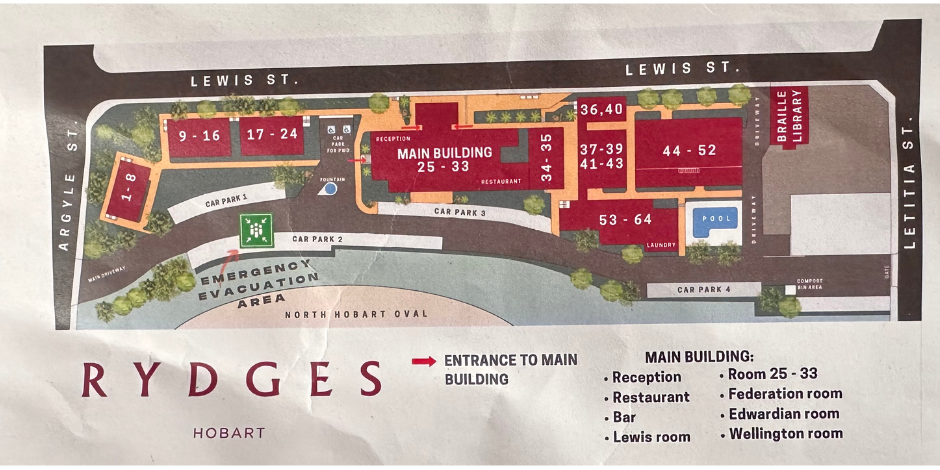
For NDIS professionals, recognising swallowing difficulties requires attention to several warning signs:
Early identification of these symptoms allows for timely referral to speech pathologists and other specialists who can perform comprehensive assessments and develop management plans.
Core Components of Dysphagia Support Training
Effective dysphagia management training for NDIS professionals covers several key areas:
Assessment awareness: While formal assessment is conducted by speech pathologists, support workers need training to recognise changes in swallowing function and understand assessment reports.
Documentation skills: NDIS requirements include detailed documentation of client care needs, interventions, and responses to ensure consistent care across all support staff.
Practical feeding techniques: Hands-on training in proper positioning, pacing, and use of specialised equipment.
Emergency response: Clear protocols for managing choking incidents and other swallowing emergencies.
Collaborative practice: Working effectively with multidisciplinary teams including speech pathologists, dietitians, and medical professionals.
Training programs should align with the NDIS high intensity support skills and combine theoretical knowledge with practical skill development through demonstrations, simulations, and supervised practice.

Best Dysphagia Treatment Protocols for Healthcare Professionals
Evidence-based dysphagia management relies on several established protocols and approaches that NDIS professionals should understand:
Modified Texture Framework: The IDDSI system provides standardised terminology and testing methods for food textures and drink thicknesses, ensuring consistent care across different settings and providers.
Compensatory Strategies: These include postural adjustments (chin tuck, head turn), swallowing manoeuvres (effortful swallow, Mendelsohn technique), and sensory enhancement methods that can immediately improve swallowing safety without requiring long-term rehabilitation.
Rehabilitation Exercises: Strength and coordination exercises for the lips, tongue, jaw, and throat muscles may improve swallowing function over time. These include tongue-hold exercises, Shaker exercises, and laryngeal range-of-motion activities.
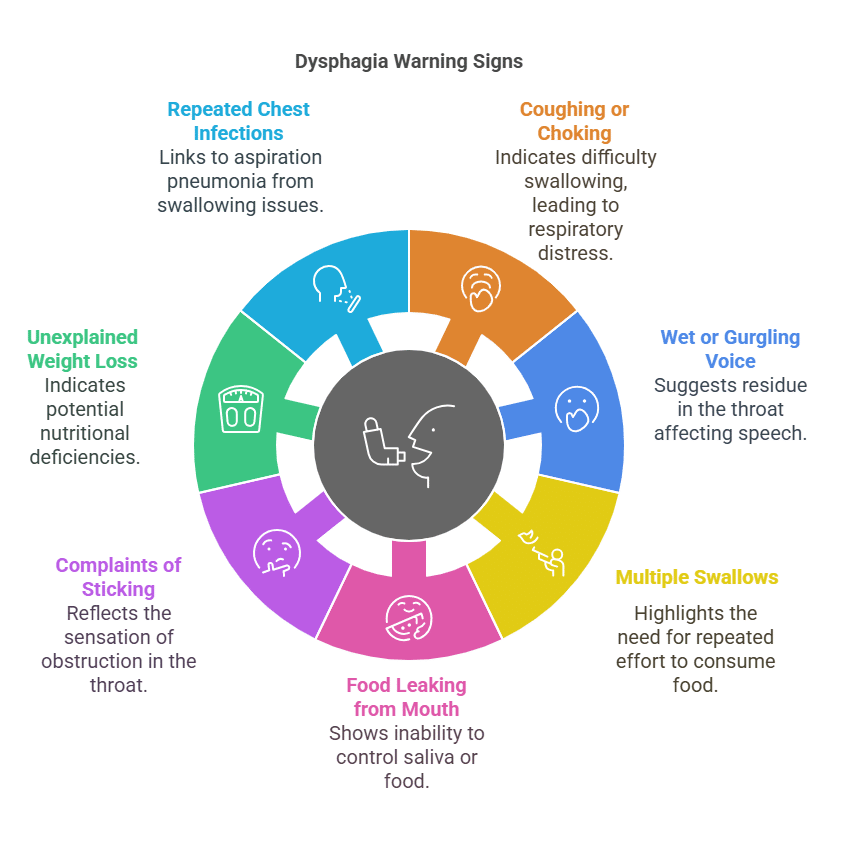
Neuromuscular Electrical Stimulation (NMES): This therapy uses small electrical currents to stimulate muscles involved in swallowing, potentially improving strength and coordination when combined with traditional therapy.
Biofeedback Approaches: Surface electromyography (sEMG) and other biofeedback tools allow clients to visualise their swallowing muscle activity, helping them make specific adjustments during therapy.
Interdisciplinary Care Planning: Best practice involves collaboration between speech pathologists, dietitians, occupational therapists, and support workers to create comprehensive management plans addressing both safety and quality of life.
NDIS professionals should be familiar with these approaches even though some interventions may only be implemented by specialists. This knowledge helps support workers understand the rationale behind specific strategies and ensure consistent implementation across all care settings.

Texture Modified Diets: Implementation and Monitoring
Understanding how to safely prepare a texture-modified diet is central to dysphagia management training. The International Dysphagia Diet Standardisation Initiative (IDDSI) framework provides globally standardised terminology and definitions for modified food textures and liquid thicknesses.
Disability support workers need practical knowledge of:
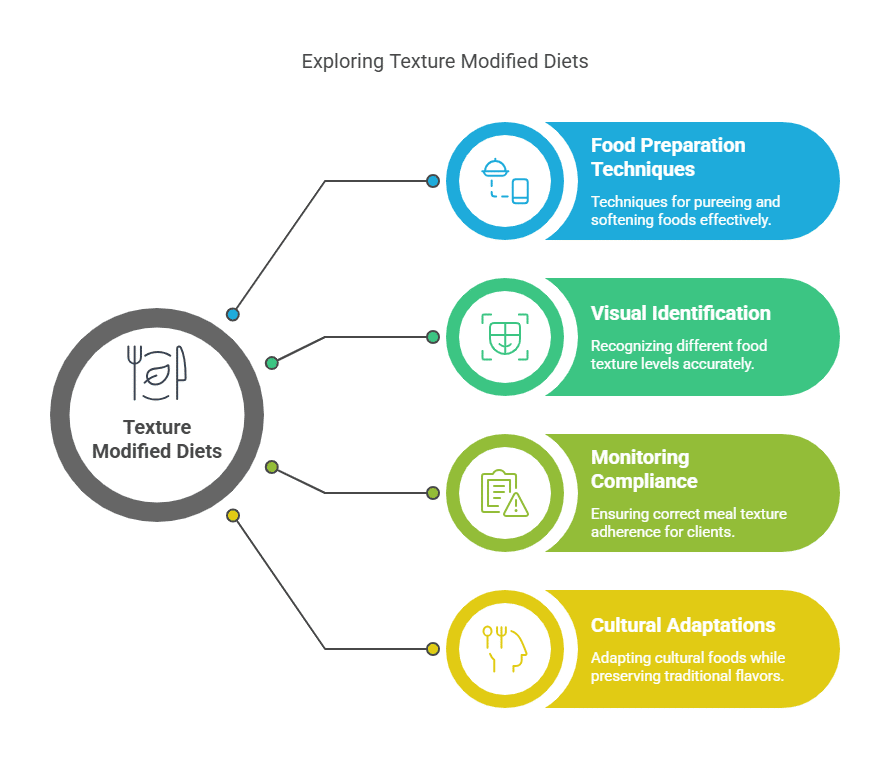
Training should include practical demonstrations of food modification techniques using commonly available equipment such as food processors, blenders, and sieves.
Thickened Liquids: Best Practices and Safety Protocols
Managing thickened liquids for dysphagia requires specific skills and attention to detail:
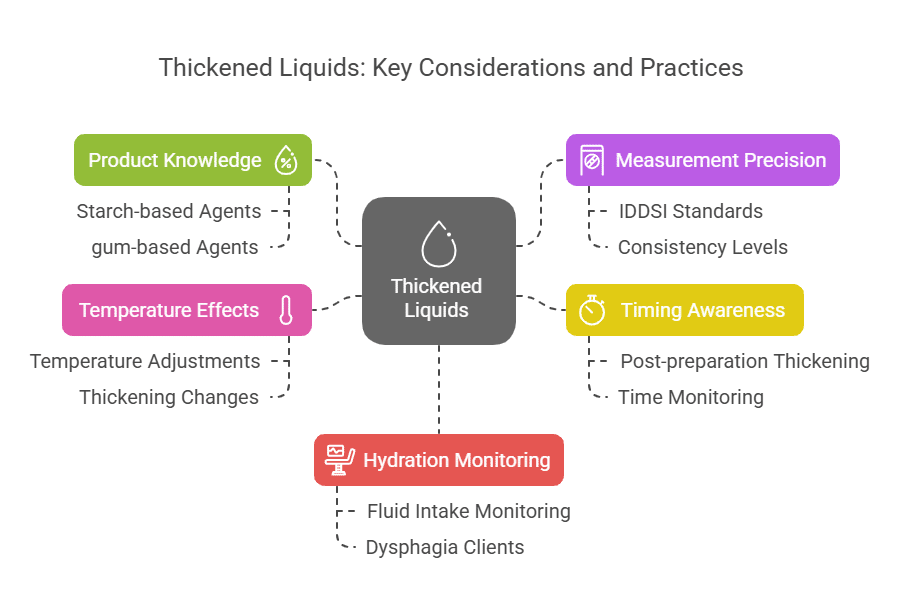
Support workers should receive hands-on practice in preparing thickened liquids to various consistencies and testing them using IDDSI flow tests.
How to Help Someone with Dysphagia Eat Safely

A critical component of dysphagia support training is learning practical feeding assistance techniques:
Optimal positioning: Proper upright posture (90-degree angle when possible) with head slightly forward.
Environmental considerations: Minimising distractions, ensuring adequate lighting, and allowing sufficient time for meals.
Pacing strategies: Offering small amounts and ensuring one swallow is complete before offering the next bite.
Visual checking: Ensuring the mouth is clear before offering more food.
Verbal cueing: Reminding clients to swallow twice per mouthful if needed.
Dignity preservation: Maintaining respectful interaction despite the need for assistance.
Training should emphasise that safe feeding is not just about preventing aspiration—it’s also about preserving dignity and making mealtimes pleasant social experiences.
High Intensity Support Skills Required by NDIS Standards
The NDIS classifies dysphagia management as a high-intensity support requiring specialised training. Key requirements include:
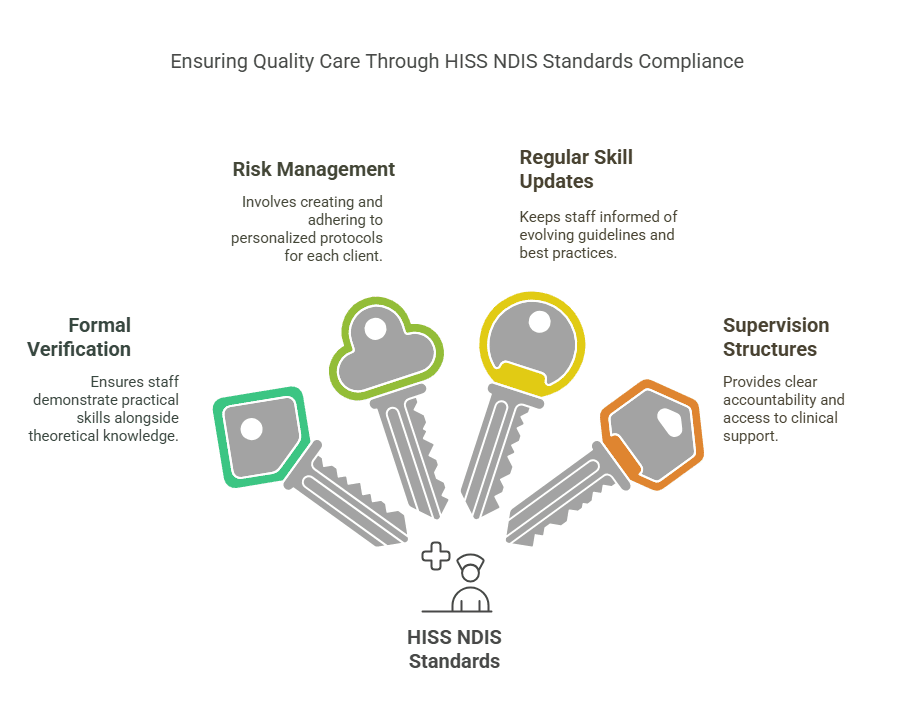
NDIS providers must ensure staff complete appropriate training programs and maintain ongoing competency verification as part of their quality assurance processes.
NDIS Quality Standards and Dysphagia Support
Dysphagia support within the high intensity support skills descriptor framework (NDIS) is governed by specific quality standards that ensure participants needing complex care receive safe, effective support. These standards include:
Practice Standard 1: Rights and Responsibilities Support workers must respect participants’ rights to make informed choices about their dysphagia management while balancing duty of care responsibilities.
Practice Standard 2: Provider Governance and Operational Management Providers must have clear policies and procedures for dysphagia management, including staff training requirements, supervision structures, and incident reporting protocols.
Practice Standard 3: Provision of Supports Dysphagia supports must be delivered according to evidence-based practice and the participant’s approved plan, with regular reviews and adjustments as needed.
Practice Standard 4: Support Provision Environment The environment for mealtime assistance must be safe, appropriate, and conducive to dignified eating experiences.
High Intensity Daily Personal Activities Module
Dysphagia management falls under this specialised module, which requires:
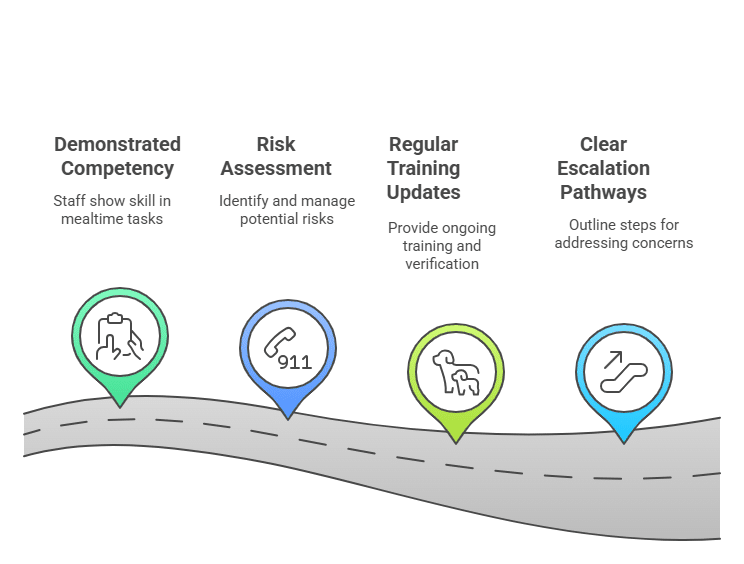
Providers must maintain evidence of staff training and competency assessments as part of their registration requirements. Regular audits may examine this documentation during quality reviews.
Measuring Training Effectiveness and Client Outcomes
Quality dysphagia support training includes methods for evaluating both staff competency and effective care outcomes:
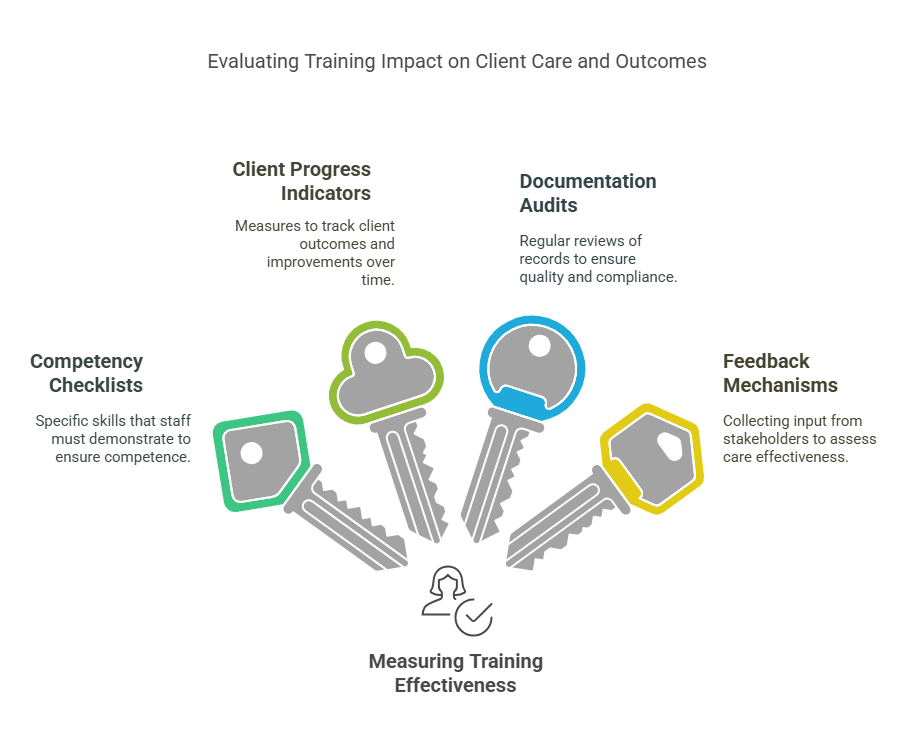
NDIS providers should implement systems to regularly review these measures and address any identified gaps in training or implementation.
Ready to demonstrate measurable competency in dysphagia support? First Aid Pro’s industry-leading Dysphagia Support Training provides you with the skills, knowledge, and confidence to deliver exceptional care that makes a real difference in clients’ lives. Enrol Today!
NDIS Recognised Dysphagia Support Training Components
Recognised NDIS support training provides comprehensive education and skill development for support workers and health professionals. A quality program covers:
Theoretical Foundations:
- Anatomy and physiology of normal swallowing
- Pathophysiology of common swallowing disorders
- Impact of various conditions on swallowing function
- Nutritional considerations for people with dysphagia
Assessment and Identification:
- Recognising early warning signs of swallowing difficulties
- Understanding clinical assessment reports
- Monitoring changes in swallowing function
- Documenting observations effectively
Practical Support Techniques:
- Positioning for safe swallowing
- Food and fluid modification according to IDDSI standards
- Safe feeding assistance methods
- Medication administration for people with dysphagia

Risk Management:
- Choking prevention strategies
- First aid response for airway blockages
- Aspiration prevention techniques
- Infection control related to dysphagia
Person-Centred Approaches:
- Maintaining dignity during mealtime assistance
- Supporting participant choice and control
- Balancing risk management with quality of life
- Cultural considerations in dysphagia management
Documentation and Communication:
- Understanding and implementing mealtime management plans
- Effective handover procedures
- Interprofessional communication
- Reporting changes and incidents
Participants completing NDIS recognised training should demonstrate practical competency in these areas through supervised practice, assessment tasks, and ongoing verification of skills.
Why Comprehensive Dysphagia Treatment Education Is Essential
Dysphagia support training is an integral component of the NDIS high intensity support skills standards. As such it is essential for NDIS professionals providing complex, client-centric care. Through proper training, support workers can confidently implement safe swallowing strategies, correctly prepare modified diets and thickened liquids, and know when to seek additional professional guidance.
The focus should always remain on person-centred approaches that balance safety with quality of life. By developing these specialised skills and meeting NDIS quality standards, health and support workers make a significant difference in the health, nutrition, and overall wellbeing of Australians living with dysphagia.