A fracture is a medical term for a break or crack in a bone and requires prompt and correct first aid to prevent further injury and reduce pain.. This can range from a small, hairline crack to a complete break where the bone is split into two or more pieces. Fractures can occur from trauma (falls, accidents), direct blows, overuse, or health conditions that weaken the bones (like osteoporosis or some cancers). Fractures may be:
- Closed: Bone is broken but the skin remains intact.
- Open (compound): Bone breaks through the skin, creating a wound and increasing the risk of infection
Whether it’s a simple closed fracture or a more serious open or compound fracture, your response could make the difference between safe recovery and long-term complications.
Be prepared. Enrol in a nationally recognised first aid course with First Aid Pro today to learn proper fracture management techniques.

Key Takeaways
- A fracture is a break or crack in a bone and requires immediate first aid.
- Use the DRSABCD protocol to manage life-threatening situations.
- Immobilise the injured limb with splints and bandages without moving it.
- Call 000 for serious fractures, especially open or compound types.
- First aid training is essential to respond correctly and calmly in emergencies.
Understanding Fractures: What You Need to Know
As discussed above, a fracture is a break, crack, or splintering of a bone caused by trauma, overuse, or underlying medical conditions. Fractures can range from minor hairline cracks to severe, life-threatening compound (open) fractures where the bone pierces the skin. They can be complete (bone broken into two or more pieces) or partial (a crack that doesn’t go all the way through the bone). Fractures can occur in any bone in your body.
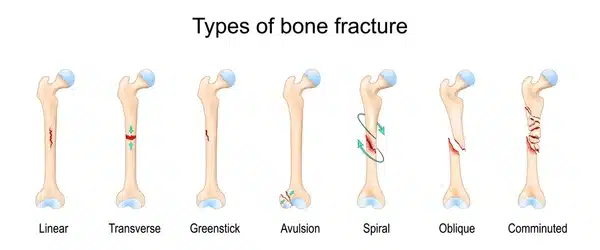
Types of Fractures
Type of Fracture | Description |
Closed Fracture | Bone breaks but skin remains intact |
Open (Compound) Fracture | Bone pierces through skin, increasing risk of infection |
Comminuted Fracture | Bone is shattered into three or more pieces |
Greenstick Fracture
Oblique
Stress (hairline) fracture | Incomplete fracture, common in children
The break has an angled pattern.
Small cracks caused by repetitive force or overuse |
Transverse | The break is in a straight line across the bone |
Understanding the type of fracture can help you apply the right first aid while waiting for professional help.
Recognising the Signs and Symptoms of a Fracture

Fractures typically occur after trauma such as falls, sports injuries, or accidents. Signs include:
- Pain at the site of injury, which may be severe and increase with movement or pressure.
- Swelling and tenderness over the affected area.
- Bruising or discolouration around the injury.
- Deformity or an unusual shape of the limb or joint—this may include a visibly out-of-place or misshapen appearance.
- Inability to move the limb normally, reduced range of motion, or loss of function.
- Difficulty or inability to put weight on the affected limb, or refusal to move it (especially in children).
- A grating sensation or sound when trying to move the limb (sometimes called “crepitus”).
- Numbness or tingling if the nerves are affected.
- Open wounds or bleeding, with bone protruding through the skin (in open fractures).
- In rib fractures, symptoms may include shallow breathing or chest pain during movement.
In more severe cases, people may also experience dizziness, faintness, or shock, particularly if there is significant blood loss or trauma.
Young children may simply refuse to use the affected limb or cry when it is touched or moved.
If you observe these signs after an injury, suspect a fracture and seek medical attention promptly. Severe symptoms such as a limb at an unusual angle, heavy bleeding, bone visible through the skin, or any signs of shock require urgent emergency care.
First Aid for Fractures

The DRSABCD Approach
If arriving on the scene of an emergency, follow the DRSABCD action plan, especially if the casualty is unresponsive or there’s a suspected head or spinal injury.
Step | Action |
D | Danger – Ensure scene is safe |
R | Response – Check for consciousness |
S | Send for help – Call Triple Zero (000) |
A | Airway – Clear and check airway |
B | Breathing – Look, listen, feel |
C | CPR – Start if not breathing |
D | Defibrillator – Apply if available |
For a suspected fracture, only proceed with immobilisation if the casualty is conscious and breathing.
Managing Pain, Swelling, and Bleeding
1. Controlling Bleeding
- Apply direct pressure: If the fracture is associated with bleeding, use a sterile dressing, clean cloth, or pad to apply firm, direct pressure to the wound. This is the most effective way to stop most external bleeding. If bone is protruding, apply pressure around (not directly over) the exposed bone.
- Cover wounds: Dress any open wounds to reduce the risk of infection.
- Embedded objects: If there is an embedded object, do not remove it. Apply pressure and dressing around the object, not on top of it.
- Bandage: Once bleeding is controlled, secure the dressing with a bandage. Avoid making bandages too tight—check circulation regularly (look for pale, cold, numb, or blue fingers/toes).

2. Managing Swelling
- Immobilise the fracture: Use a splint or sling in the position found to prevent movement and further injury.
- Apply ice: Apply an ice pack (wrapped in a cloth) to the injured area for 15–20 minutes at a time. Repeat every few hours if needed. Do not apply ice directly to the skin.
- Elevate: Elevate the injured limb above the level of the heart if possible, unless this causes more pain or is not advised (such as with certain leg fractures). This helps reduce swelling.
3. Managing Pain
- Keep the person still and comfortable: Reduce movement to limit pain and further damage.
- Over-the-counter pain relief: If safe and appropriate, paracetamol or ibuprofen can be given for pain. Do not give medication if the injured person is allergic, unable to swallow, or has been advised not to by a healthcare professional.
- Ice application: As above, ice not only reduces swelling but can temporarily numb the area and help manage pain.
- Monitor vital signs: Watch for signs of shock (such as pale, clammy skin, rapid pulse, or faintness) and treat if needed.
Immobilising the Injured Limb: Splints and Support
Fractured limbs must be immobilised to prevent further damage. Here’s how:
| How to Apply a Splint | |
|---|---|
| 1 | Do not attempt to straighten the bone. |
| 2 | Support the limb in the position found. |
| 3 | Use a rigid item (stick, ruler, rolled newspaper) as a splint. |
| 4 | Wrap the splint using a bandage above and below the fracture site. |
| 5 | Pad the splint well to avoid pressure points. |
| 6 | Check circulation every 15 minutes. |
| TIP | Tip: Ensure bandages are not too tight. Watch for signs of loss of circulation: pale or blue fingers/toes, numbness, or cold skin. |
Be confident in your first aid. Join a First Aid Pro course today and get hands-on training in fracture and emergency care.

When to Seek Medical Assistance
Always seek urgent medical help when:
- There is a suspected open or compound fracture
- The limb appears deformed or immobile
- The fracture involves the head, neck, spine, or rib
- Bleeding cannot be controlled
- Pain is severe and unrelieved
Call Triple Zero (000) and request an ambulance for any serious or life-threatening injury.
Special Considerations: Sprains, Dislocations, and Rib Fractures

Sprains:
- Immediate Management: Most mild sprains benefit from the RICE protocol (Rest, Ice, Compression, Elevation). However, current Australian resources suggest not to use ice directly on the skin.
- Stabilisation: For moderate to severe cases, physiotherapists may advise bracing, taping, or bandaging for several weeks. External supports are chosen based on injury severity, healing phase, patient needs, and pain levels.
- Exercise & Rehabilitation: Once acute inflammation subsides, guided rehabilitation is crucial, focusing on restoring strength, flexibility, and balance to prevent recurrence. Early physiotherapy intervention is recommended for severe sprains.
- Risks & Prevention: History of previous injuries, poor joint strength or flexibility, and inadequate footwear increase risk. Preventive taping/bracing is beneficial for previous injuries.
- Special Populations: Older adults may experience slower recovery and higher risk for complications.

Dislocations
- Emergency First Aid: Do not attempt to relocate the joint yourself. Immobilise the joint in the position found, use padding/splints or a sling for limbs, and apply a cold pack (never directly on skin) to reduce swelling and pain.
- When to Seek Urgent Care: Always seek emergency care if severe pain, obvious deformity, loss of pulse, nerve involvement (numbness, bluish skin), or inability to move joint occurs.
- Reduction: Closed reduction (by professionals) is the standard of care for most dislocations, followed by short-term immobilisation (sling or splint, usually 1–3 weeks for the shoulder). Never attempt reduction yourself due to risk of nerve, vessel, or fracture complications.
- Imaging: Pre- and post-reduction X-rays (sometimes CT/MRI) assess for fractures or concurrent injuries, especially in complex dislocations or recurrence.
- Rehabilitation: Early, supervised mobilisation is preferable over prolonged immobilisation to maintain range of motion and reduce chronic instability. Gradual strengthening and specific functional exercises are required before return to sport or strenuous activity.
- Recurrence Risk & Surgical Consideration: Young, active individuals—especially males—are at high risk of recurrence after shoulder dislocation. Surgery may be indicated for repeated dislocations or associated injuries.
- Joint-Specific Points:
- Shoulder: External rotation immobilisation may reduce recurrence; evidence is stronger in younger patients (<40 years).
- Patella (Knee Cap): Avoid casting; use splints allowing movement. Early physiotherapy and weightbearing help recovery.
- Finger/Elbow: Conservative treatment is usually preferred; early mobilisation is emphasised unless there are instability or neurovascular concerns.
- Patient Education: Stress the importance of completing rehab and recognising early signs of instability to avoid further injuries.

Rib Fractures
- Initial Assessment: Assess for associated injuries—such as pneumothorax, hemothorax, and pulmonary contusion—which may require urgent intervention.
- Pain Management: Adequate analgesia is crucial to allow effective breathing and coughing, reducing the risk of pneumonia. Multimodal pain strategies (oral, localized, nerve blocks) may be needed.
- Respiratory Support & Activity: Encourage deep breathing, coughing, and ambulation to prevent atelectasis and respiratory complications. Avoid bedrest as much as possible.
- Red Flags for Emergency Referral: Indications include worsening shortness of breath, low oxygen saturation (<92%), intractable pain, suspected internal organ injury, or signs of shock.
- Surgical Fixation (SSRF): Surgical stabilisation is increasingly considered, especially for chest wall instability (flail chest), three or more displaced rib fractures, and patients unable to wean from ventilation. Early operation (<72 hours) is favoured when indicated and when no contraindications exist.
- Special Populations: Elderly and comorbid patients (e.g., COPD, obesity) are at heightened risk for complications and may need more intensive monitoring and support.
- Follow-Up: Persistent pain, cough, fever, or breathing issues after discharge should prompt review to exclude delayed complications
Infection Control in Open Fractures
Use sterile dressings from your first aid kit and avoid contaminating the wound. Do not touch the exposed bone. Wear disposable gloves if available.
Item | Purpose |
Sterile dressing | Cover and protect open wound |
Triangular bandage | Immobilise limb or support arm |
Gauze and tape | Control bleeding and secure dressings |
Recovery, Monitoring, and Rehabilitation
After emergency treatment:
- The hospital may apply a cast, brace, or perform surgery.
- Recovery time depends on the type and severity of the fracture.
- Physio may be required to regain strength and mobility.
- Monitor for infection, especially after compound fractures.
Take the next step—enrol with First Aid Pro and equip yourself with certified first aid skills for any emergency.
References
- Better Health Channel: Bone Fractures
- Safe Work Australia – First Aid in the Workplace
- HealthyWA (WA Dept of Health): First Aid for fractures & Dislocations
- Royal Children’s Hospital Melbourne: Fractures (Broken Bones)