As common as broken bones are, most people aren’t fully prepared to handle this emergency when it strikes.
Medically, a fracture describes any disruption in the normal integrity of a bone. This can range from a thin crack to a complete break, and the bone may fracture crosswise, lengthwise, in several places, or into many pieces.
Understanding the proper first aid techniques for fractures can mean the difference between a smooth recovery and potential long-term complications.

Key Takeaways
- Recognise signs of broken bones: deformities, swelling, severe pain, and loss of function in the affected area.
- Immediately assess the scene for safety, evaluate the victim’s condition, and call for professional medical help.
- Immobilise the injured area using splints, padding joints above and below the fracture site to prevent further damage.
- Manage pain and shock by elevating the limb, applying cold therapy, and providing emotional support to the patient.
- Seek immediate medical attention for open fractures, severe pain, visible deformity, or inability to move the affected area.

Recognising Fractures
When performing a visual inspection, look for obvious deformities or misalignment of the affected limb or body part. You’ll often notice swelling and bruising around the injury site, which can be indicators of a fracture.
In some cases, you might observe an open wound where the bone has pierced the skin, known as a compound fracture. Listen for any grating or popping sounds when the injured area moves, as this can indicate bone fragments rubbing together.
Remember that not all fractures are immediately apparent. If you suspect a broken bone, it’s important to immobilise the affected area and seek professional medical attention promptly. X-rays and other imaging techniques will be necessary for a definitive diagnosis.
Types of Fractures

In your first aid knowledge, understanding the types of fractures is essential.
Common Fracture Classifications
The most basic classification distinguishes between open (compound) and closed fractures. Further classifications include complete fractures, where the bone separates entirely, and incomplete fractures, such as greenstick fractures in children, where the bone partially breaks.
Fracture types can also be categorised by their pattern. Transverse fractures occur perpendicular to the bone’s long axis, while oblique fractures angle across the bone. Spiral fractures result from twisting forces, and comminuted fractures involve multiple bone fragments. Impacted fractures occur when bone fragments are driven into each other.
Additionally, fractures may be classified as displaced or non-displaced, depending on whether the bone fragments have moved out of alignment. Understanding these classifications is essential for proper diagnosis and treatment planning.
Open Vs. Closed Fractures
Open fractures, also known as compound fractures, occur when the broken bone penetrates the skin, creating an open wound. These injuries are more severe due to the increased risk of infection and tissue damage.
Closed fractures, on the other hand, don’t break the skin. While they’re generally less severe than open fractures, they can still cause significant internal damage.
Immediate First Aid For Fractures

When responding to a potential broken bone situation, your first priority is to assess and secure the scene.
Assess and Secure Scene
Scene safety is paramount; you can’t assist effectively if you become a casualty yourself. Conduct a thorough environmental assessment, scanning for:
- Ongoing threats (e.g., traffic, unstable structures)
- Hazardous materials or conditions
- Potential for further injury to the victim or responders
Check Victim’s Condition
Begin by checking the victim’s level of consciousness. If they’re responsive, ask about their pain level and location. If unresponsive, immediately check for breathing and pulse.
Perform a quick head-to-toe examination, looking for visible injuries, deformities, or signs of bleeding. Pay close attention to the area where the suspected broken bone is located. Don’t move the victim unless absolutely necessary to prevent further injury.
Check essential signs, including respiratory rate, pulse, and skin colour. Rapid, shallow breathing or an irregular pulse may indicate shock. Cool, pale, or clammy skin is another sign of shock that requires immediate attention.
Assess for other injuries that may be masked by the pain of the broken bone. Look for signs of internal bleeding, such as bruising or swelling. If the victim is conscious, ask about any numbness, tingling, or loss of sensation, which could indicate nerve damage.
Immobilisation Techniques
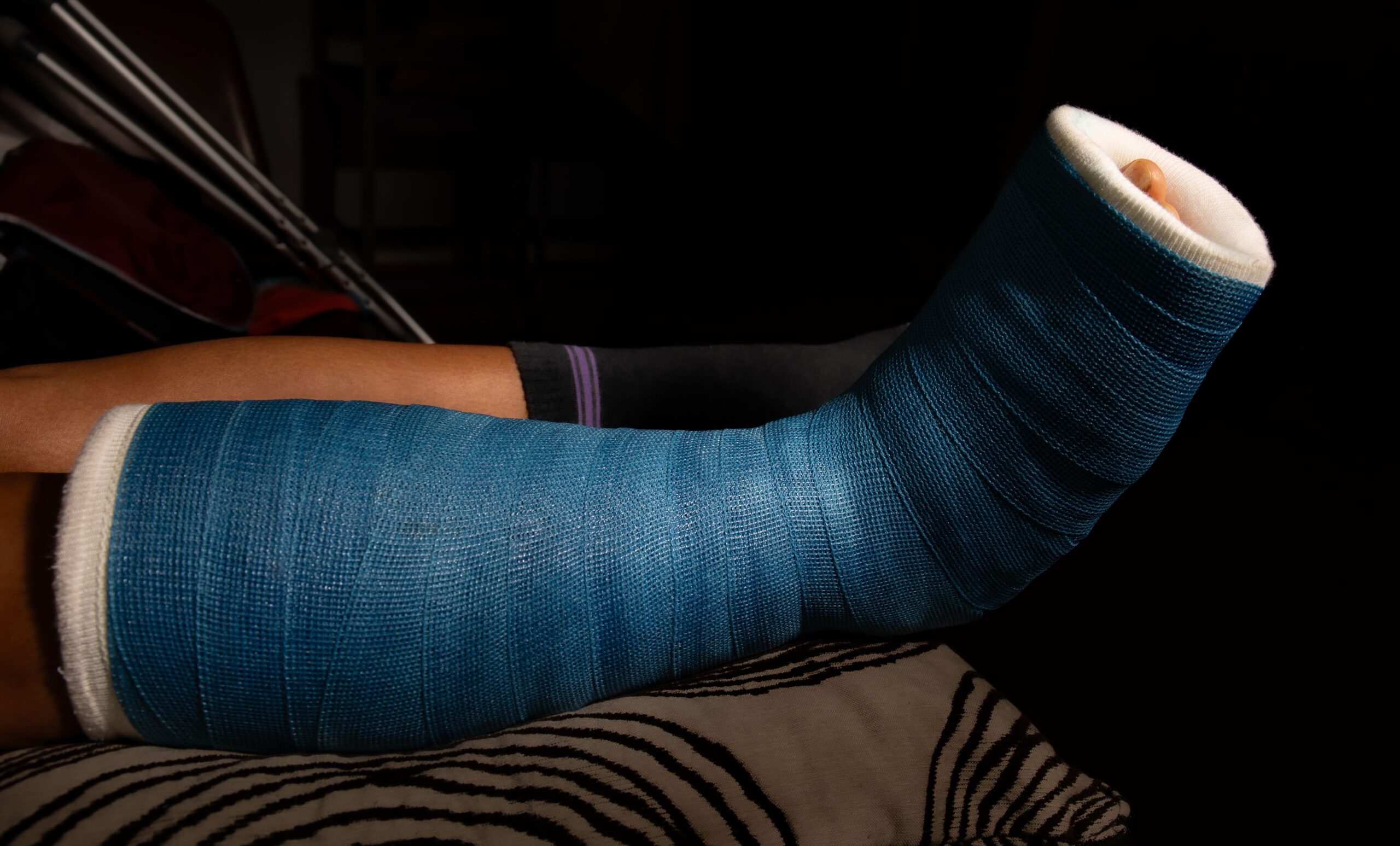
Proper immobilisation of a fractured bone is essential to prevent further injury and alleviate pain during first aid treatment. When dealing with a suspected fracture, your primary goal is to stabilise the affected area using appropriate techniques and available materials.
For limb fractures, improvised splints can be highly effective. You’ll need to:
- Immobilise the joint above and below the fracture site
- Use rigid materials like boards, rolled newspapers, or cardboard for support
- Pad the splint to prevent pressure points and additional discomfort
Preventing Shock
Recognising shock symptoms is vital when dealing with broken bones.
Recognise Shock Symptoms
Key indicators of shock include pale, cool, and clammy skin, rapid and shallow breathing, and a weak, rapid pulse. Monitor the patient’s level of consciousness, as confusion or disorientation may signal worsening shock.
Shock causes include considerable blood loss, severe pain, and the body’s stress response to trauma. To aid in shock prevention, take these essential steps:
- Maintain the patient’s body temperature by covering them with blankets
- Keep the patient lying flat on their back with legs elevated, if possible
- Loosen tight clothing to promote circulation
Immediate Shock Management Techniques
Begin by laying the patient flat on their back and elevating their legs about 30 centimetres, unless this position causes pain or further injury. Cover them with a blanket to prevent heat loss, an important shock prevention strategy.
Monitor the patient’s breathing and pulse regularly. If they’re conscious, encourage them to take slow, deep breaths to increase oxygen intake. Don’t give them anything to eat or drink, as this could lead to complications if emergency surgery is required.
Employ emotional support techniques to keep the patient calm and reassured. Speak in a soothing voice, explain what you’re doing, and provide constant reassurance. This can help reduce anxiety and potentially mitigate the severity of shock.
When to Seek Medical Help

You should seek professional help when you experience severe pain, visible deformity, or inability to move the affected area. These symptoms indicate fracture urgency and require prompt evaluation by medical professionals.
Don’t hesitate to call emergency services or visit the nearest emergency department if you notice:
- Bone protruding through the skin (open fracture)
- Severe bleeding or swelling around the injury site
- Loss of sensation or circulation in the affected limb
Complications of Broken Bones
Broken bones, despite often being viewed as straightforward injuries, can occasionally lead to serious complications that you’ll need to be aware of and monitor closely.
One of the most urgent complications is compartment syndrome, where swelling causes pressure to build up in the affected limb, potentially cutting off blood supply. You’ll need to watch for severe pain, numbness, or a pale, cool limb.
Another serious issue is fat embolism, where fat globules enter the bloodstream and can cause breathing difficulties or even stroke-like symptoms.
Infection is a risk, especially with open fractures. You’ll need to monitor for signs such as fever, increased pain, or discharge from the wound site.
Long-term effects can include chronic pain, arthritis, or reduced mobility in the affected area. In children, growth plate injuries can lead to uneven limb growth.
Less common but still significant complications include malunion (improper healing alignment), delayed union, or non-union (failure to heal). These may require additional medical intervention, including surgery, to correct.
Recovery and Rehabilitation
Recovery from a bone fracture typically involves three key phases: inflammation, repair, and remodelling. During these stages, your body works to heal the broken bone and restore its strength. The recovery timeline varies depending on the severity and location of the fracture, but it generally ranges from 6 to 12 weeks for most simple fractures.
Rehabilitation exercises play an important role in your recovery. These exercises are tailored to your specific injury and may include gentle stretching, strength training, and balance activities. It’s vital to follow your healthcare provider’s instructions carefully and not rush the process, as this could lead to re-injury or prolonged recovery.
Throughout your rehabilitation, you’ll likely undergo regular check-ups and imaging tests to monitor your progress. As you regain strength and mobility, your healthcare provider will gradually increase the intensity of your exercises.
Frequently Asked Questions
How can I tell the difference between a fracture and a sprain?
Fractures typically cause intense, focused pain, possible cracking sounds during injury, visible deformity, rapid bruising, and inability to use the affected limb. Sprains usually allow limited movement, cause less swelling, and rarely show visible deformity. Only medical imaging can confirm a fracture definitively.
What should I do if I suspect a spinal or neck fracture?
Do not move the person unless they’re in immediate danger. Call emergency services immediately. Keep the person completely still, supporting their head and neck in the position found without straightening or adjusting. If movement is absolutely necessary due to danger, move the entire body as a single unit with multiple helpers. Monitor breathing and consciousness while awaiting professional help.
Is it safe to apply ice directly to a suspected fracture?
No, never apply ice directly to the skin over a suspected fracture. Always wrap ice packs in a thin towel before application. Apply cold for 15-20 minutes, then remove for at least 40 minutes before reapplying. Stop immediately if the person reports increased pain or numbness. Use caution with individuals who have circulatory problems or reduced sensation.