Hypovolaemia, also known as hypovolemia, is a condition where the body does not have enough blood or fluid circulating, which can lead to hypovolaemic shock—a life-threatening medical emergency. This article explains the causes, symptoms, stages, and emergency first aid for hypovolaemia, with practical advice aligned to Australian first aid standards.
Be ready to act when seconds matter. Enrol in a nationally recognised first aid course with First Aid Pro today and learn the skills that save lives.

Key Takeaways
Hypovolaemia (hypovolemia) is a condition where the body does not have enough circulating blood or fluid, which can quickly lead to hypovolaemic shock, a life-threatening medical emergency.
Causes include severe bleeding (haemorrhagic shock), fluid loss from diarrhoea, vomiting, dehydration, or burns, and certain medical conditions.
Symptoms of hypovolaemic shock range from thirst, weakness, and rapid heartbeat in early stages, to confusion, low blood pressure, and collapse in severe cases.
First aid for shock in Australia follows DRSABCD: call 000, control bleeding, lay the person flat, elevate legs if safe, keep them warm, and monitor until paramedics arrive.
Medical treatment requires urgent care in hospital, with IV fluids, blood transfusions, and sometimes surgery to stop internal bleeding.
Prevention includes staying hydrated, using safety measures to avoid trauma, and ensuring workplaces and communities have trained first aiders.
What is Hypovolemia?
Hypovolaemia (sometimes spelled hypovolemia) refers to an abnormal decrease in blood volume, either from losing blood or losing fluids. Without enough circulating blood or fluid, the heart cannot pump effectively, blood pressure drops, and vital organs become starved of oxygen.
When hypovolemia progresses, it results in hypovolaemic shock, a life-threatening condition requiring immediate medical attention. Unlike milder dehydration, hypovolemia is defined by significant loss of circulating blood volume, which may come from bleeding, burns, diarrhoea, or other causes.
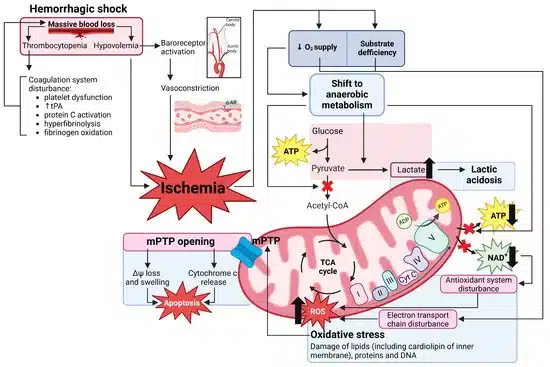
Pathophysiology of Hypovolemic Shock
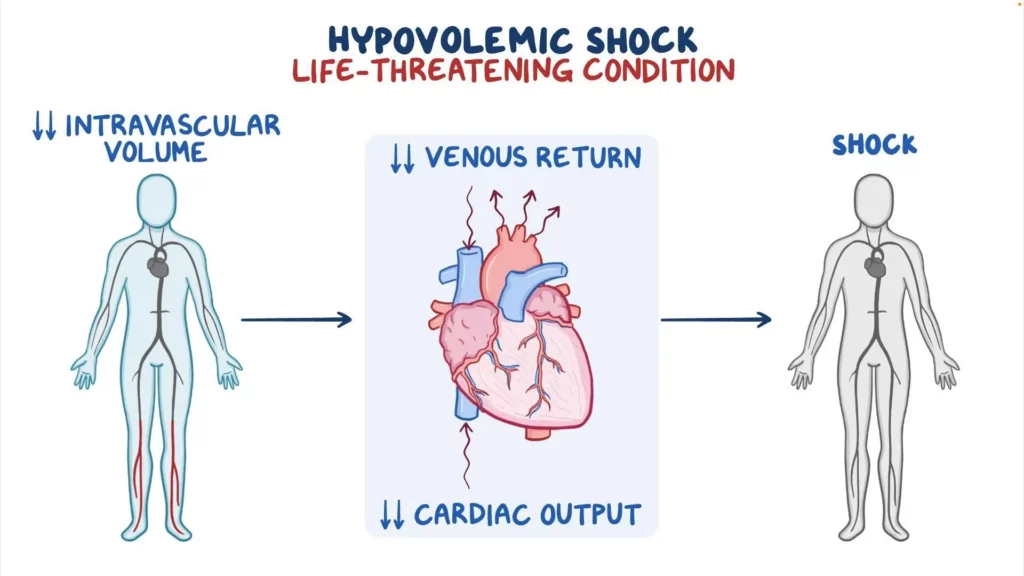
Hypovolemia reduces blood flow to organs, causing tissue hypoxia and triggering compensatory mechanisms such as increased heart rate and vasoconstriction. If untreated, it can rapidly progress to shock and organ failure.
The pathophysiology of hypovolaemic shock is straightforward but severe. When blood or fluid is lost:
- Preload falls: Less blood returns to the heart.
- Cardiac output drops: The heart cannot pump enough blood.
- Blood pressure declines: Vessels constrict to maintain perfusion.
- Organ perfusion fails: Kidneys, brain, and heart suffer from reduced oxygen.
Without immediate treatment, organ damage occurs quickly. Shock is a life-threatening condition and must always be treated as a medical emergency.
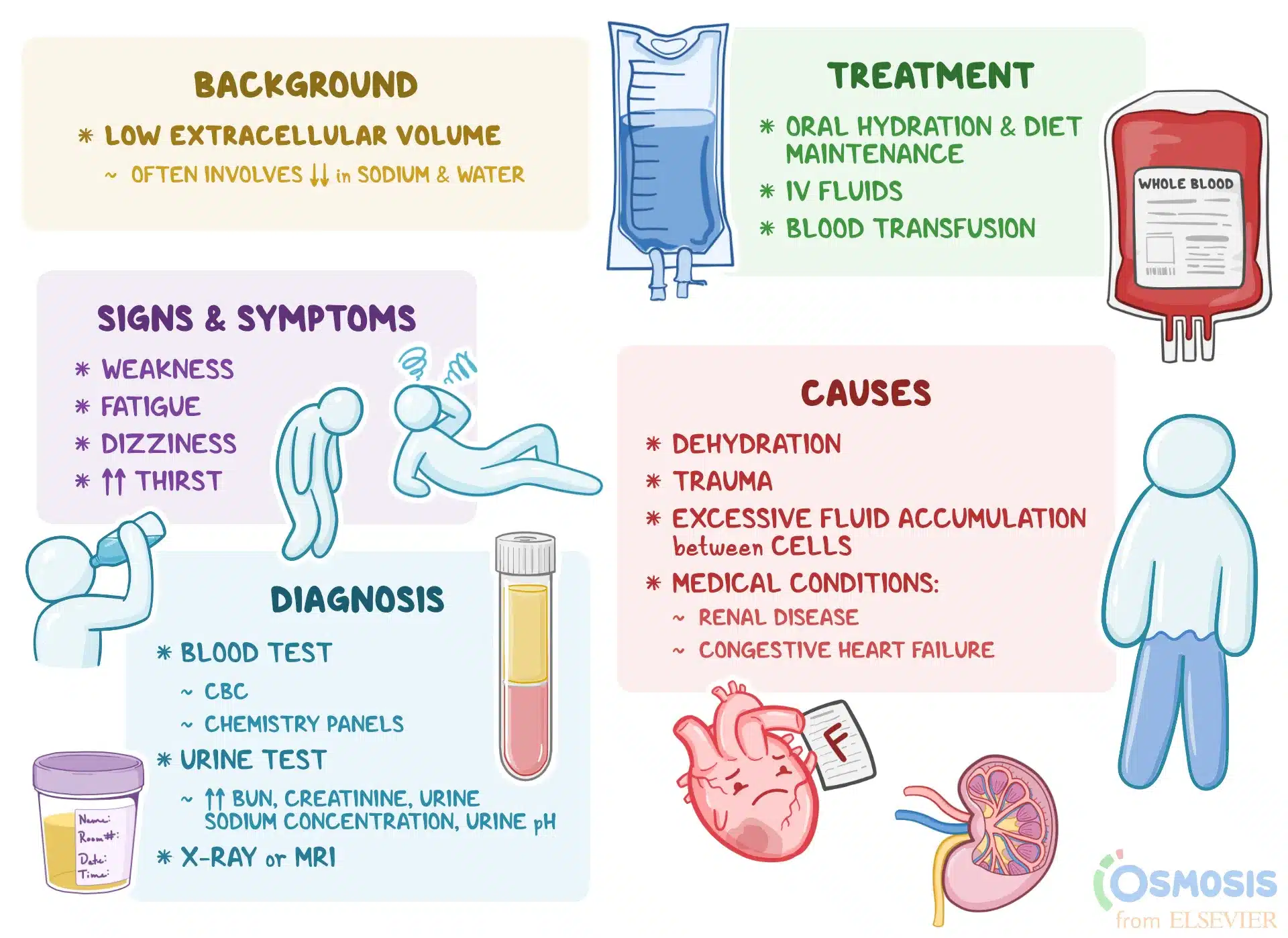
Symptoms and Causes of Hypovolemia
Causes of Hypovolemic Shock
The most common causes of hypovolemia include:
- Haemorrhage (haemorrhagic shock): Severe external or internal bleeding from trauma, accidents, surgery, or gastrointestinal bleeding.
- Fluid loss without bleeding: Severe diarrhoea, vomiting, heatstroke, and burns can all cause dangerous fluid loss.
- Other medical conditions: Sepsis, renal problems, or uncontrolled diabetes can worsen fluid depletion.
Symptoms of Hypovolemic Shock
Early recognition is crucial. Symptoms of hypovolemia include:
- Weakness and dizziness
- Rapid heart rate (tachycardia)
- Pale, clammy skin
- Low blood pressure
- Confusion, agitation, or fainting
As hypovolemia worsens, severe hypovolaemic shock may present with:
- Extremely low blood pressure
- Very weak or absent pulse
- Rapid, shallow breathing
- Cold extremities
- Loss of consciousness
Stages of Hypovolemic Shock
Doctors and first aid texts often describe stages of hypovolaemic shock based on the percentage of blood loss.
Stage | Amount of Blood/Fluid Lost | Vital Signs | Clinical Signs |
Class I | < 15% blood volume | Normal BP, slight ↑HR | Mild thirst, pale skin |
Class II | 15–30% blood volume | HR > 100 bpm, ↓pulse pressure | Anxiety, rapid breathing |
Class III | 30–40% blood volume | BP falls, HR > 120 bpm | Confusion, weak pulse, cold skin |
Class IV | > 40% blood volume | Severe hypotension, HR > 140 bpm | Lethargy, collapse, organ failure |
Shock is a medical emergency. If someone may be experiencing shock, call 000 in Australia immediately.
Signs and Symptoms Associated with Hypovolemic Shock
Early / Compensated Stage
- Rapid heart rate (the heart compensates for fluid loss)
- Thirst and weakness (classic early symptoms of hypovolaemia)
Progressive Stage
- Low blood pressure (not enough fluid to circulate)
- Cold, clammy skin (blood vessels constrict)
- Confusion or agitation (brain not getting oxygen)
Severe / Decompensated Stage
- Reduced urine output
- Blue lips or fingertips (poor oxygen circulation)
- Collapse or loss of consciousness
Hypovolemic Shock vs Dehydration
It’s important to distinguish between dehydration and hypovolemia. While dehydration refers to general fluid loss, hypovolemia specifically means circulating blood volume is too low.
First Aid for Shock
First aid for shock follows the DRSABCD protocol recommended by the Australian Resuscitation Council.
DRSABCD – Key Steps
Protocol-
D
Danger – ensure the area is safe.
-
R
Response – check if the person is conscious.
-
S
Send for help – call 000 immediately.
-
A
Airway – clear and maintain an open airway.
-
B
Breathing – check for normal breathing.
-
C
CPR – start CPR if not breathing.
-
D
Defibrillation – apply an AED if available.
Specific Shock First Aid Actions
Immediate-
1
Lay the person flat (supine). Do NOT raise the legs unless advised by advanced care or in special circumstances.
-
2
Control severe external bleeding with firm, direct pressure.
-
3
Keep the person warm (use a blanket; never apply direct heat), reassure them, and monitor for changes.
Be prepared for real emergencies. Join a First Aid Pro course to learn how to provide lifesaving first aid care for shock and hypovolemia.
Medical Management and Treatment
Once in the emergency department, treatment for hypovolemia depends on the cause:
- IV fluids (intravenous fluids): Saline or Ringer’s lactate to restore circulating volume.
- Blood transfusions: For major haemorrhage or trauma.
- Surgical intervention: To stop internal bleeding.
- Oxygen therapy and monitoring: In an intensive care unit if severe.
Hypovolaemic shock is a life-threatening condition. Prompt treatment in hospital is essential to prevent organ damage and death.
Types of Shock
For context, hypovolaemic shock is one type of shock, but not the only one:
- Hypovolaemic shock – from blood or fluid loss.
- Cardiogenic shock – the heart cannot pump effectively.
- Obstructive shock – obstruction blocks blood flow (e.g., pulmonary embolism).
- Septic shock – overwhelming infection causes vessel dilation and fluid loss.
- Anaphylactic shock – allergic reaction causes vessel dilation and fluid leakage.
Understanding these differences helps explain why hypovolaemic shock must be treated rapidly and specifically with fluid or blood replacement.

Preventing Hypovolemia
- Use seatbelts and workplace safety equipment to prevent traumatic bleeding.
- Stay hydrated in hot Australian climates to reduce risk of fluid loss.
- Manage chronic medical conditions with medical support.
- Know first aid for shock and ensure workplaces have trained first aiders.
Don’t wait until an emergency strikes. Enrol in a First Aid Pro course and be ready to act when someone’s life is on the line.
Hypovolemia & Hypovolaemic Shock — Recognise Early, Act Fast
Hypovolemia—whether from blood loss or severe fluid loss—can progress rapidly to hypovolaemic shock, a life-threatening condition where vital organs are starved of oxygen due to insufficient circulating blood volume. Early recognition matters: watch for rapid heart rate, pale clammy skin, dizziness, confusion and low blood pressure, and treat any visible bleeding immediately. In Australia, follow DRSABCD, call 000, lay the person flat (do not raise the legs unless advised), keep them warm, and monitor closely until help arrives.
Building strong first aid capability is the most reliable way to turn knowledge into confident action. If you’d like practical training aligned with Australian guidelines, enrol in a nationally recognised first aid course with First Aid Pro and be ready to respond when seconds count.
Knowledge Test Quiz: Hypovolaemia & Shock
Test your understanding of hypovolaemia and shock.
References
Cleveland Clinic. Hypovolemia and Hypovolemic Shock.
Better Health Channel (Vic Govt). Shock – Causes, Symptoms and Treatment.
Healthdirect Australia. Shock – Symptoms and First Aid.