Pain management in first aid involves systematic assessment and treatment techniques used by trained first aiders to reduce suffering and improve patient outcomes in workplace and community emergency situations. Effective pain relief in first aid settings combines non-pharmacological methods like cold therapy, elevation, and immobilisation with appropriate medication administration, all while ensuring safety and recognising when to access professional medical help.
Understanding how to manage pain effectively is crucial for anyone providing first aid, whether in workplace environments, community settings, or emergency situations. The ability to recognise different types of pain, assess severity accurately, and apply suitable treatment methods can significantly improve a patient’s quality of life during critical moments before professional medical care arrives.
Ready to advance your first aid skills? First Aid Pro offers nationally recognised PUAEME008 Provide Pain Management courses across Australia. Our comprehensive training covers workplace safety requirements and advanced pain management techniques for first aiders. Register today to enhance your emergency response capabilities.

Key Takeaways
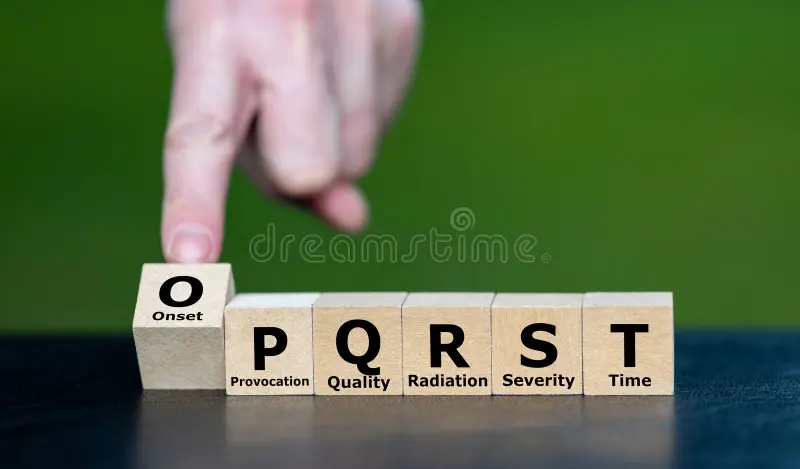
- Assessment First: Always conduct systematic pain assessment using OPQRST before implementing any treatment strategies. Accurate assessment guides appropriate intervention and helps identify medical emergencies requiring immediate professional care.
- Non-Drug Options: Cold therapy, elevation, compression, and immobilisation provide effective first-line pain management without medication risks. These techniques should be attempted before or alongside pharmacological interventions.
- Medication Safety: Understand paracetamol vs ibuprofen indications, contraindications, and proper dosing guidelines. Always check for allergies, existing medical conditions, and potential drug interactions before administration.
- Know Your Scope: Recognise when pain requires emergency services (000) or advanced medical care. Red flag symptoms include altered consciousness, signs of shock, or severe pain unresponsive to basic interventions.
- Document Everything: Maintain detailed records of pain scores, treatments administered, and patient responses. Proper documentation ensures continuity of care and protects both patient and provider.
When Pain Management in First Aid is Necessary
Using OPQRST and Pain Assessment Scales
Proper pain assessment forms the foundation of effective pain management in first aid. Before administering any treatment, first aiders must systematically evaluate the patient’s condition to ensure appropriate care and identify potential medical emergencies requiring immediate ambulance assistance.
OPQRST Pain Assessment Technique
Use this structured approach to explore a patient’s pain history to guide safe, effective first aid.
| Component | Questions to Ask | Why It Matters |
|---|---|---|
| O Onset | When did the pain start? Was it sudden or gradual? | Helps identify acute vs chronic conditions |
| P Provocation | What makes it better or worse? | Guides treatment decisions |
| Q Quality | How would you describe the pain? sharp dull burning | Indicates potential injury type |
| R Radiation | Does the pain spread anywhere else? | May reveal serious underlying conditions |
| S Severity | Rate your pain from 0–10. | Determines urgency and treatment approach |
| T Timing | Is it constant or intermittent? | Affects medication timing and effectiveness |
Tip: For Severity, use the 0–10 numeric rating scale (0 = no pain, 10 = worst imaginable). Reassess after interventions (e.g., rest, ice, immobilisation) to monitor change.
This systematic assessment helps first aiders make informed decisions about treatment while providing valuable information to paramedics and medical professionals during handover.
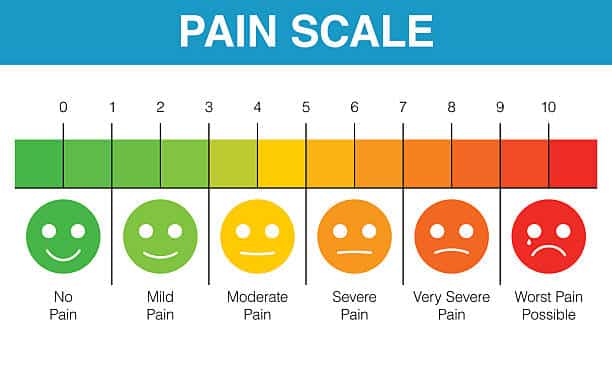
Pain Scale 0–10 First Aid Applications
The numeric rating scale is the most widely used pain assessment tool in first aid situations. Patients rate their pain from 0 (no pain) to 10 (worst imaginable pain), providing a standardised measure that healthcare professionals can track over time.
Pain Scale Guidelines:
- 0-3: Mild pain – usually manageable with basic first aid techniques
- 4-6: Moderate pain – may require medication and non-pharmacological interventions
- 7-10: Severe pain – often requires emergency medical attention and advanced pain management
For unconscious patients or those unable to communicate, first aiders should observe behavioural indicators including facial expressions, body positioning, vital signs changes, and vocal responses to assess pain levels.

Non-Pharmacological Pain Relief First Aid Techniques
Many effective pain management strategies don’t involve medication, making them ideal for workplace first aid situations where drug administration may be restricted or inappropriate. These techniques can provide immediate relief while reducing the risk of complications.
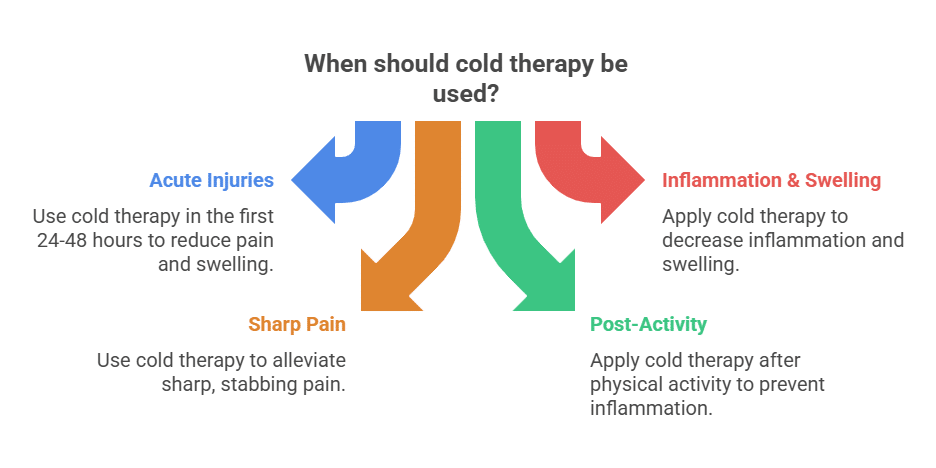
Cold Pack for Pain First Aid Management
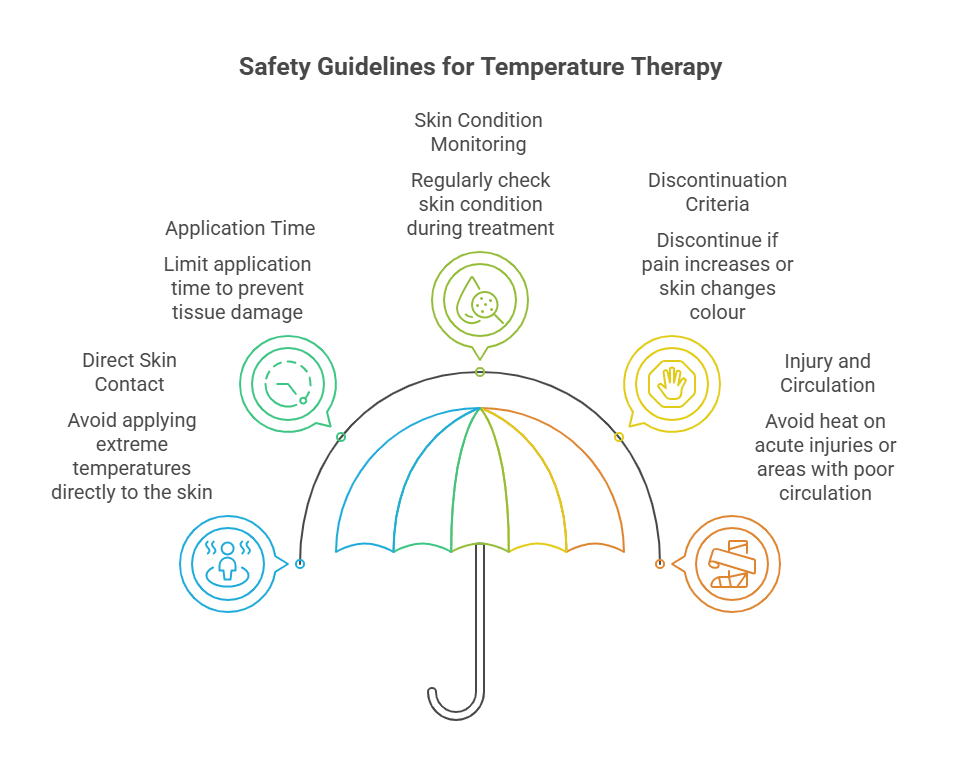
Cold therapy remains one of the most effective non-pharmacological pain relief methods available to first aiders. Proper application can significantly reduce pain, swelling, and inflammation in acute injuries.
Cold Therapy Application:
- Apply within the first 15-20 minutes after injury
- Use commercial cold packs or ice wrapped in a thin towel
- Apply for 15-20 minutes every 2-3 hours for first 24-48 hours
- Never apply ice directly to skin to prevent frostbite
- Check circulation regularly during application
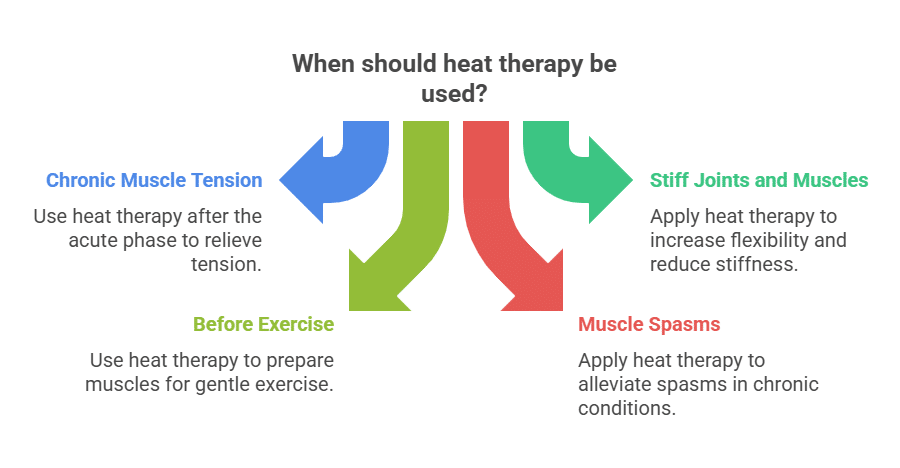
When to Use Cold vs Heat: Cold therapy is appropriate for acute injuries, inflammation, and swelling. Heat therapy should only be used for chronic muscle tension or after the acute inflammatory phase (usually after 48-72 hours). Ensure you consult appropriate medical advice when uncertain.
Elevation to Reduce Pain and Swelling
Elevating an injured limb above the level of the heart uses gravity to reduce blood flow to the injury site, thereby decreasing swelling and associated pain. This technique works particularly well for extremity injuries and should be combined with other pain management strategies.
Proper Elevation Technique:
- Position the injured area above heart level when possible
- Support the limb comfortably using pillows or soft materials
- Ensure circulation isn’t compromised
- Monitor for changes in colour, temperature, or sensation
- Maintain elevation for extended periods when practical

Compression Bandage for Pain Control
Appropriate compression can reduce swelling, provide support to injured tissues, and subsequently decrease pain levels. However, improper technique can compromise circulation and worsen the patient’s condition.
Compression Guidelines:
- Apply firm, even pressure without restricting blood flow
- Use appropriate bandage width for the injury site
- Start distal (furthest from heart) and work proximally
- Check circulation every 15-20 minutes
- Look for signs of compromised blood flow: blue/grey skin colour, coldness, numbness

Immobilisation First Aid: Splinting for Pain Relief
Immobilising injured areas prevents further damage and significantly reduces pain by limiting movement. This technique is particularly effective for suspected fractures, severe sprains, and joint injuries.
Basic Splinting Principles:
- Splint above and below the injury site
- Use rigid materials when available (boards, magazines, rolled newspapers)
- Pad bony prominences to prevent pressure sores
- Secure firmly but allow for swelling
- Check circulation, sensation, and movement regularly
For upper limb injuries, slings provide excellent support while allowing some mobility. Ensure the sling supports the weight of the arm without putting excessive pressure on the neck.

RICE vs PEACE & LOVE Soft-Tissue Injuries Protocol
Understanding both traditional and modern approaches to soft-tissue injury management ensures first aiders can apply the most appropriate and evidence-based techniques for optimal patient outcomes.
Traditional RICER First Aid Method
The RICER protocol has been widely taught in first aid training for decades and remains relevant for immediate injury management:
- Rest: Cease activity to prevent further injury
- Ice: Apply cold therapy to reduce inflammation
- Compression: Apply appropriate pressure to limit swelling
- Elevation: Raise injured area above heart level
- Referral: Seek appropriate medical assessment
While RICER remains effective for immediate injury management, recent studies suggest that prolonged rest may actually impede recovery in some cases.
Modern PEACE & LOVE Approach
Current best practice for soft-tissue injury care—immediate steps (PEACE) followed by active recovery (LOVE).
PEACE (Immediate Care)
-
P
Protect
Unload or restrict movement for 1–3 days to limit aggravation.
-
E
Elevate
Elevate the limb above heart level to help reduce swelling.
-
A
Avoid Anti-inflammatories Caution
They may impair tissue healing in the early phase; seek clinical advice before use.
-
C
Compress
Apply external mechanical pressure (e.g., elastic bandage) to limit oedema and pain.
-
E
Educate
Explain the condition, expected recovery, and self-management strategies to support informed choices.
LOVE (Ongoing Management)
-
L
Load
Gradually return to normal activities as symptoms allow; use pain as a guide.
-
O
Optimism
A positive outlook is associated with better outcomes and adherence to rehab.
-
V
Vascularisation
Introduce pain-free cardiovascular activity early to promote healing.
-
E
Exercise
Progress mobility, strength, and functional exercises to restore full capacity.
Notes: Protect briefly—then reintroduce symptom-guided loading. Seek medical care for severe pain, deformity, or red-flag symptoms. In an emergency, call 000.
This approach emphasises active recovery while respecting the natural healing process, leading to better long-term outcomes for many patients.
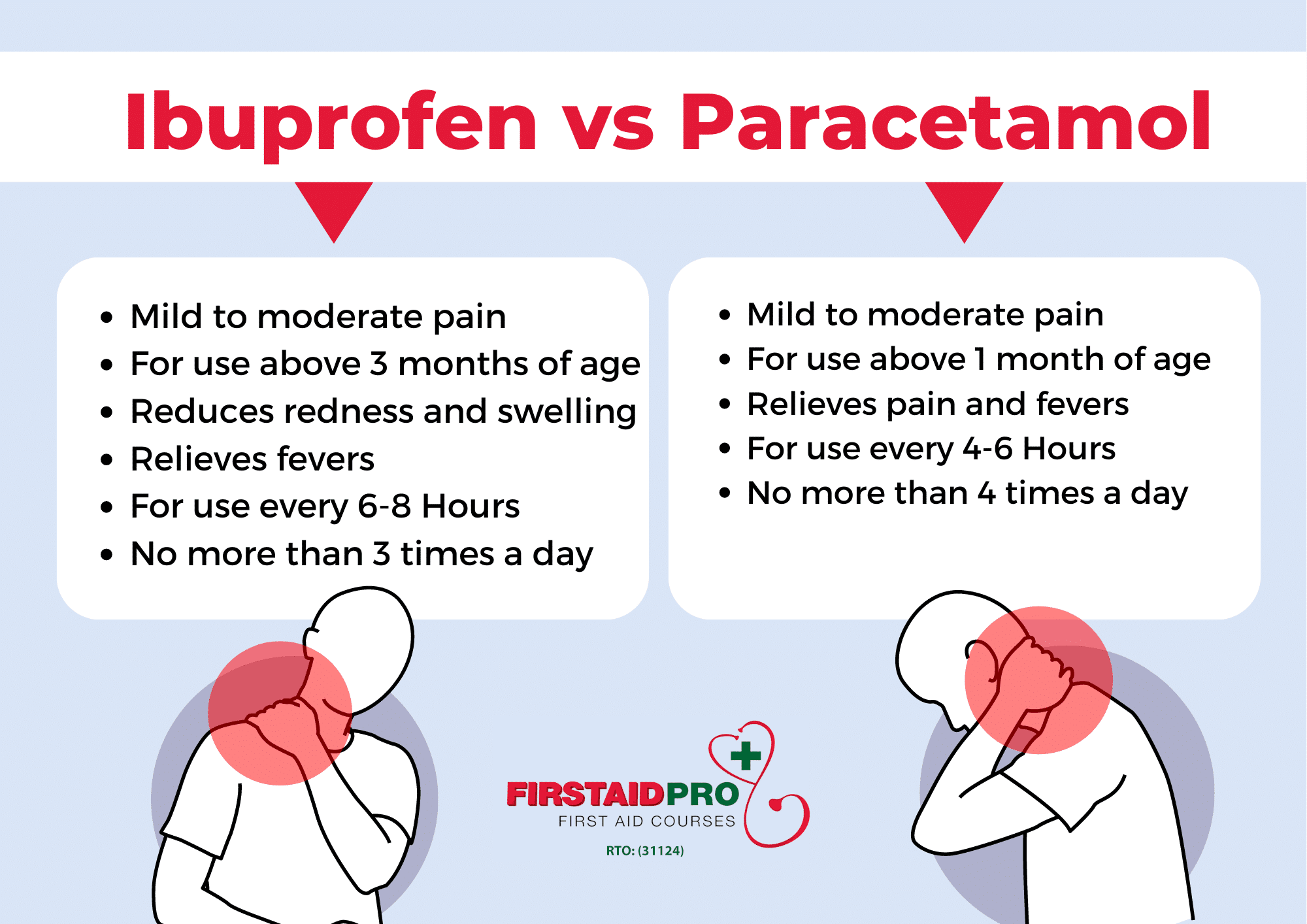
Paracetamol vs Ibuprofen: Australian First Aid Guidelines
First aiders in workplace and community settings often need to decide between different over-the-counter pain medications. Understanding the differences between paracetamol and ibuprofen ensures safe and effective treatment while reducing the risk of adverse reactions.
Paracetamol First Aid Applications
First-line option for mild–moderate pain in many first-aid situations due to a strong safety profile and broad effectiveness.
Paracetamol Advantages
-
✓
Suitable for most age groups
From 1 month of age with appropriate dosing and formulation.
-
✓
Fewer drug interactions
Generally fewer interactions than many other analgesics.
-
✓
Compatible with many conditions
Often suitable alongside common medical conditions (check individual advice).
-
✓
Effective for common pains
Headaches, muscle pain, and general discomfort.
-
✓
Multiple formulations
Tablets, liquid, and suppositories to suit age and circumstance.
Dosing Guidelines
Adults Max 4,000 mg / 24 h
| Dose | Frequency | Daily Maximum |
|---|---|---|
| 500–1,000 mg | Every 4–6 hours | 4,000 mg (24 hours) |
Children Weight-based Max 60 mg/kg / 24 h
| Dose | Frequency | Daily Maximum |
|---|---|---|
| 10–15 mg/kg per dose | Every 4–6 hours | 60 mg/kg (24 hours) |
Important Always check the medication packaging for specific instructions and formulation strength. Safety Never exceed the recommended daily maximums to prevent liver damage.
Notes: Paracetamol is called acetaminophen in some countries. Follow label directions and seek pharmacist/GP advice if unsure, for infants, pregnancy, liver disease, or if pain persists. In an emergency, call 000.
Enhance your pain management expertise: First Aid Pro’s PUAEME008 course covers advanced medication administration techniques for qualified first aiders. Learn about restricted analgesics, proper documentation, and workplace safety requirements. Enrol now to expand your first aid capabilities.

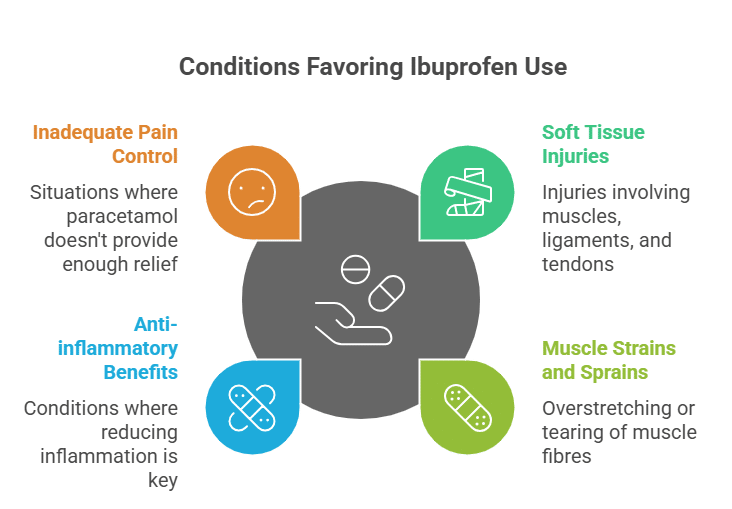
Ibuprofen First Aid Use and Precautions
Ibuprofen belongs to the non-steroidal anti-inflammatory drug (NSAID) class and offers both pain relief and anti-inflammatory effects, making it particularly useful for injuries involving inflammation.
Dosage Summary Table
Medication | Adults | Children (6+ months) | Maximum Daily Dose |
Paracetamol | 500-1000mg every 4-6 hours | 10-15mg/kg every 4-6 hours | Adults: 4000mg<br>Children: 60mg/kg |
Ibuprofen | 200-400mg every 6-8 hours | 5-10mg/kg every 6-8 hours | Adults: 1200mg<br>Children: 30mg/kg |
Children Pain Relief First Aid Considerations
Administering pain medication to children requires special attention to dosing, consent, and age-appropriate techniques. Always seek parental consent when possible and maintain detailed records of any medication given.
Paediatric Pain Management Considerations:
- Weight-based dosing is more accurate than age-based dosing
- Liquid formulations often preferred for children under 12
- Consider non-pharmacological methods first
- Monitor closely for adverse reactions
- Ensure medications are specifically formulated for children
- Never give adult-strength medications to children
Pain Management in First Aid for Specific Injuries
Different types of injuries require tailored approaches to pain management. Understanding how to modify techniques based on injury type ensures optimal patient comfort and outcomes.
Pain Management in First Aid for Sprains and Strains
Soft tissue injuries are among the most common workplace and sporting injuries requiring first aid intervention. Effective pain management in first aid can prevent complications and promote faster recovery.
Acute Management Strategy
Immediate care steps, followed by red-flag warnings that require urgent medical attention.
Strategy (First Aid)
-
1
Immediate assessment
Use the OPQRST method to structure the pain history.
-
2
Apply PEACE protocol
For the first 24–48 hours after soft-tissue injury.
-
3
Combine techniques
Cold therapy + elevation + compression to limit pain and swelling.
-
4
Monitor circulation
Check capillary refill, skin colour, warmth, and sensation when using compression Re-check regularly
-
5
Document response
Record pain levels (0–10) and treatment response to guide next steps.
-
6
Plan referral
Arrange appropriate GP/physio or urgent care based on severity and progress.
Warning Signs – Seek Emergency Care
-
!
Severe, unrelenting pain
Pain that doesn’t respond to initial first-aid measures.
-
!
Loss of sensation or movement
Numbness, tingling, weakness, or inability to move the limb.
-
!
Compromised circulation
Pale/blue skin, coldness, delayed capillary refill, or swelling that worsens.
-
!
Suspected fracture or dislocation
Deformity, crepitus, or bone end visibility—immobilise and seek urgent care.
-
!
Other concerning symptoms
E.g., chest pain, shortness of breath, fainting, fever, or signs of infection.
Notes: If red-flag symptoms are present, call 000 or attend emergency care. Reassess regularly and update documentation after each intervention.

Heat vs Cold for Pain: When to Use Each
Temperature therapy can be highly effective for pain management when applied appropriately. However, using the wrong type at the wrong time can worsen injuries and delay healing.

Advanced Pain Management in First Aid: Restricted Analgesics
Some first aid situations may require advanced pain management techniques using restricted analgesics. These medications require special training, certification, and careful administration protocols.
Methoxyflurane Green Whistle (Penthrox) Overview
Methoxyflurane, commonly known as the “green whistle,” is an inhaled analgesic available to trained first aiders under specific circumstances. This medication provides rapid-onset pain relief for moderate to severe pain.
PUAEME008 Provide Pain Management Requirements:
- Nationally recognised training program
- Competency assessment in safe administration
- Understanding of indications and contraindications
- Knowledge of emergency protocols
- Regular skill maintenance and updates
Methoxyflurane Characteristics:
- Onset: Pain relief within 2-3 minutes
- Duration: Effective for 25-30 minutes per device
- Administration: Self-administered under supervision
- Indications: Moderate to severe pain from trauma
- Contraindications: Respiratory depression, certain medical conditions

Entonox Analgesia Training Requirements
Entonox (nitrous oxide/oxygen mix) represents another advanced pain management option requiring specialised training. This medication provides effective pain relief while maintaining patient consciousness and protective reflexes.
Training Components:
- Physiological effects and mechanisms of action
- Proper equipment setup and maintenance
- Patient selection and contraindications
- Administration techniques and monitoring
- Emergency management and complications
- Documentation and legal requirements
First aiders interested in providing advanced pain management should consider pursuing additional qualifications through registered training organisations like First Aid Pro, ensuring they meet all regulatory requirements and maintain appropriate insurance coverage.
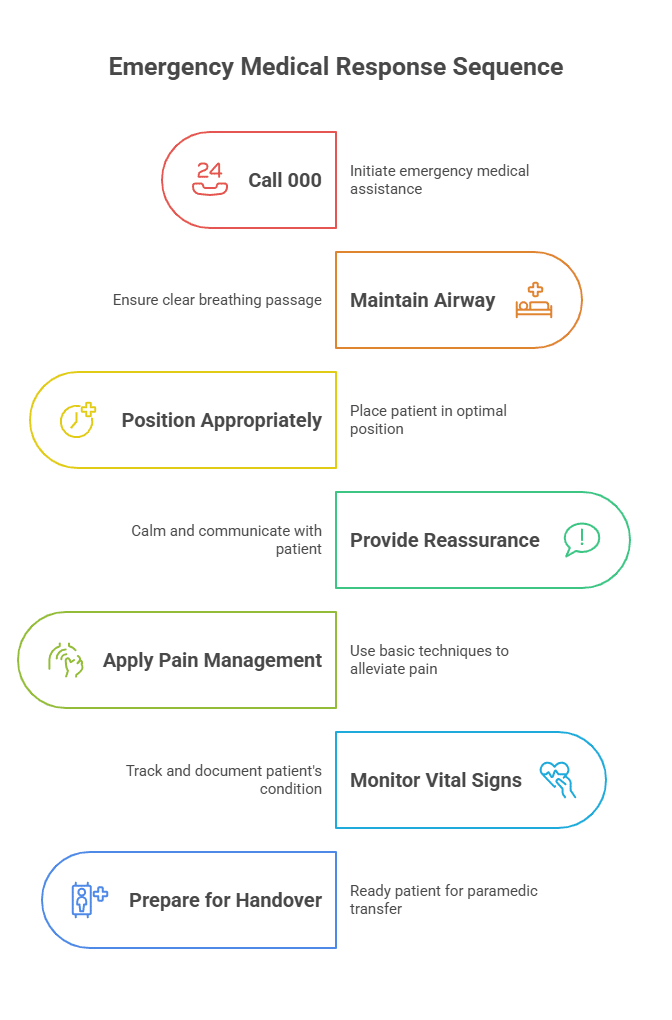
When to Call 000 for Severe Pain: Red Flag Symptoms
Recognising when pain indicates a medical emergency requiring immediate ambulance response is crucial for preventing serious complications and ensuring appropriate patient outcomes.
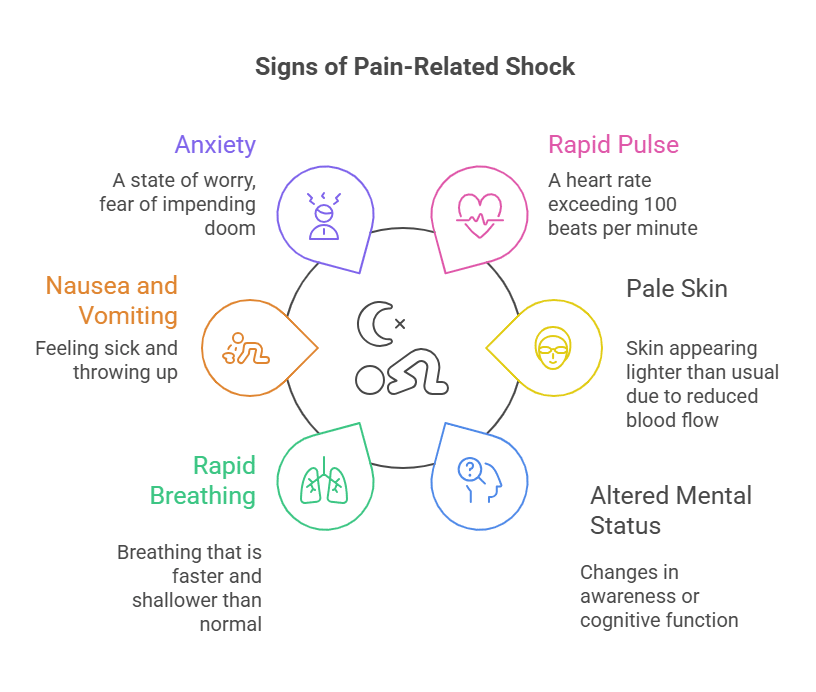
Shock and Severe Pain First Aid Recognition
Severe pain can trigger physiological shock responses that may be life-threatening. First aiders must recognise these signs and respond appropriately while managing the patient’s pain.
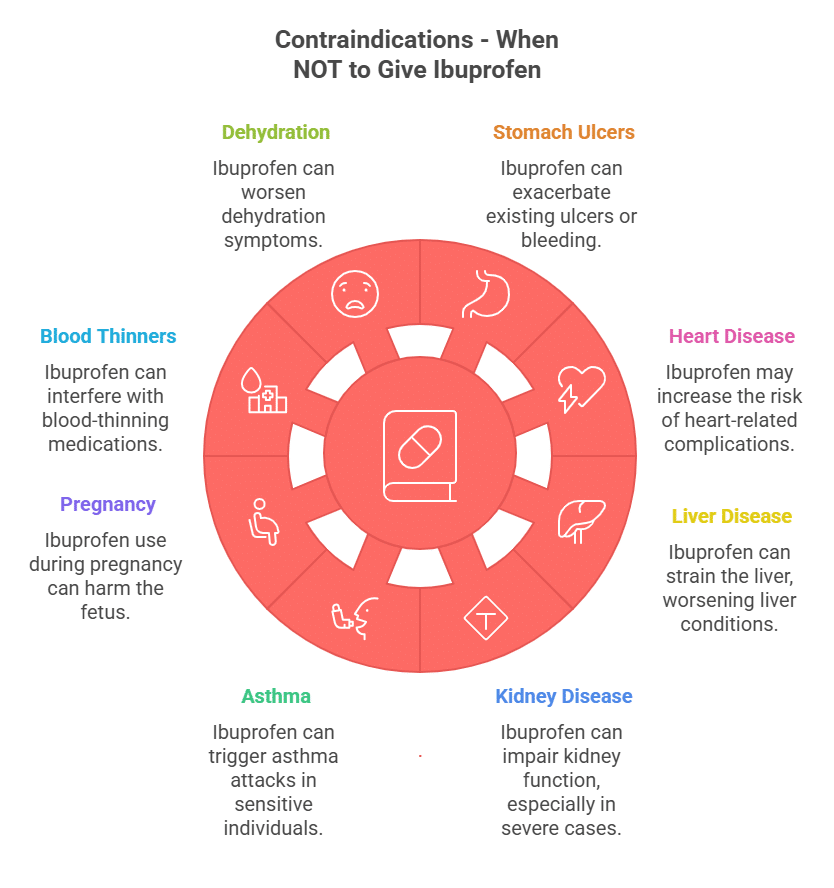
Pain Relief Contraindications First Aid Providers Must Know
Understanding when NOT to administer pain relief is as important as knowing when and how to provide it. Certain medical conditions, medications, and circumstances require alternative approaches or immediate medical referral.
Contraindications for Pain Medications
Use this quick reference to identify when pain medicines should be avoided or used with caution in first aid.
Absolute Contraindications
-
!
Known allergies to specific medications
Do not administer if the person has a documented allergy or past severe reaction.
-
!
Unconscious patients (without advanced training)
No oral medications; manage airway/breathing and seek urgent help.
-
!
Suspected internal bleeding
Avoid NSAIDs; they may worsen bleeding risk—seek medical care promptly.
-
!
Severe respiratory depression
Urgent assessment required; monitor airway, breathing, circulation.
-
!
Signs of drug or alcohol intoxication
Avoid sedating/contraindicated medicines; prioritise safety and medical evaluation.
Relative Contraindications (Use with Caution)
-
⚠
Pregnancy
Especially when pregnancy status is unknown—seek pharmacist/GP advice.
-
⚠
Chronic medical conditions
Kidney, liver, or heart disease can alter risk/benefit—check suitability first.
-
⚠
Current prescription medications
Consider interactions and duplicate dosing with combination products.
-
⚠
Age extremes
Very young or elderly may require adjusted doses/forms and closer monitoring.
-
⚠
Uncertain diagnosis or mechanism
If the cause of pain is unclear, avoid masking symptoms—seek clinical advice.
Notes: Follow product labels and local first aid protocols. When in doubt, consult a pharmacist/GP. For emergencies or red-flag symptoms, call 000.
Master advanced pain management: First Aid Pro’s PUAEME008 training covers restricted analgesics, legal requirements, and workplace safety protocols. Our experienced instructors provide hands-on training with the latest equipment and techniques. Book your course today and become qualified to provide advanced pain management in first aid.
Knowledge Test Quiz
Test your understanding of first aid pain management. Select one option for each question, then choose Check answers.
References
- Better Health Channel. Pain Relief Medications. Australian Government Department of Health.
- Australian and New Zealand Committee on Resuscitation (ANZCOR). (2024). First Aid Guidelines.
- Better Health Channel. (2024). First Aid and Emergency Care. Victorian State Government.
- Therapeutic Goods Administration (TGA). (2024). Australian Register of Therapeutic Goods. Australian Government Department of Health.
- Training.gov.au. (2024). PUAEME008 – Provide Pain Management. Australian Government Department of Employment and Workplace Relations.
- Dubois, B., & Esculier, J. F. (2019). Soft-tissue injuries simply need PEACE and LOVE. British Journal of Sports Medicine, 54(2), 72-73.
- Bleakley, C., McDonough, S., & MacAuley, D. (2004). The use of ice in the treatment of acute soft-tissue injury. American Journal of Sports Medicine, 32(1), 251-261.